Factors associated with adverse outcomes in Cameroonian patients with traumatic brain injury: A cross-sectional study
Factors Associated with Adverse Outcomes in Cameroonian Patients with Traumatic Brain Injury: A Cross-sectional Study
Friday, April 21, 2023

Samantha Sadler, BS (she/her/hers)
Medical Student
Harvard Medical School
ePoster Presenter(s)
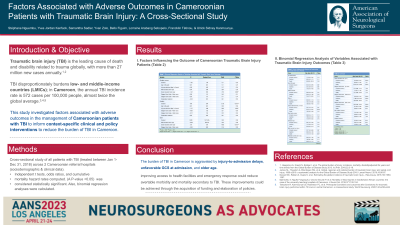
Introduction: The burden of traumatic brain injury (TBI) disproportionately affects low- and middle-income countries. In Cameroon, the estimated annual incidence rate is 572 cases per 100,000 people. This study investigated factors associated with adverse outcomes in the management of Cameroonian patients with TBI.
Methods: This cross-sectional study included all TBI patients treated between January 1 and December 31, 2018, at two Cameroonian referral hospitals. Sociodemographic and clinical data were extracted from patient charts and admission registries and analyzed with SPSS v.26. Independent T-tests, odds ratios, and cumulative mortality hazard rates were computed. A P- value < 0.05 was considered statistically significant. Also, binomial regression analyses were calculated.
Results: One hundred seventy-one patients aged 38.63 ± 20.46 years old received treatment for TBI. Most patients were male (78.9%), Cameroonian (98.2%), from urban areas (75.4%), and uninsured (88.8%). The average admission length was 11.23 ± 10.71 days, during which 27.5% of patients received surgical treatment while 72.5% received non-surgical (conservative) management. From post-discharge day 12 onwards, surgically-treated patients had a greater cumulative mortality hazard rate than conservatively-treated patients. By 28 days post- discharge, 66.1% of patients had recovered completely [Glasgow Outcome Scale (GOS)=5], 23.4% had a disability (GOS=2-4), and 10.5% expired (GOS=1). Complete recovery was associated with the absence of severe TBI (B=-1.42, SE=0.52, P=0.006), disability was associated with increased injury-to-admission delay (B=-1.27, SE=0.48, P=0.009), and death was associated with severe TBI (B=3.16, SE=0.73, P< 0.001).
Conclusion : We identified factors associated with unfavorable outcomes among Cameroonian TBI patients. These results can inform triage and referral practices and aid policymakers in developing context-specific prehospital guidelines.
Methods: This cross-sectional study included all TBI patients treated between January 1 and December 31, 2018, at two Cameroonian referral hospitals. Sociodemographic and clinical data were extracted from patient charts and admission registries and analyzed with SPSS v.26. Independent T-tests, odds ratios, and cumulative mortality hazard rates were computed. A P- value < 0.05 was considered statistically significant. Also, binomial regression analyses were calculated.
Results: One hundred seventy-one patients aged 38.63 ± 20.46 years old received treatment for TBI. Most patients were male (78.9%), Cameroonian (98.2%), from urban areas (75.4%), and uninsured (88.8%). The average admission length was 11.23 ± 10.71 days, during which 27.5% of patients received surgical treatment while 72.5% received non-surgical (conservative) management. From post-discharge day 12 onwards, surgically-treated patients had a greater cumulative mortality hazard rate than conservatively-treated patients. By 28 days post- discharge, 66.1% of patients had recovered completely [Glasgow Outcome Scale (GOS)=5], 23.4% had a disability (GOS=2-4), and 10.5% expired (GOS=1). Complete recovery was associated with the absence of severe TBI (B=-1.42, SE=0.52, P=0.006), disability was associated with increased injury-to-admission delay (B=-1.27, SE=0.48, P=0.009), and death was associated with severe TBI (B=3.16, SE=0.73, P< 0.001).
Conclusion : We identified factors associated with unfavorable outcomes among Cameroonian TBI patients. These results can inform triage and referral practices and aid policymakers in developing context-specific prehospital guidelines.
