The Accessibility and Appeal of an Online Social Support Community for Underrepresented Pediatric Epilepsy Surgery Candidates
Friday, April 21, 2023

Amani Carson, BA (she/her/hers)
Medical Student
David Geffen School of Medicine at the University of California Los Angeles
Los Angeles, California, United States
ePoster Presenter(s)
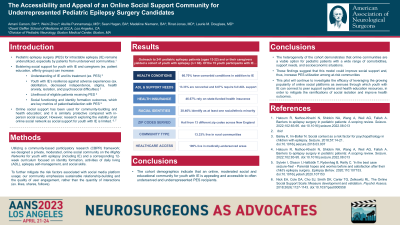
Introduction: Despite the demonstrated importance of early intervention for intractable epilepsy (IE); pediatric epilepsy surgery (PES) remains underutilized, especially among patients of color and from under-resourced communities. The existing literature suggests that bolstering social support for youth with IE and caregivers can increase the likelihood of eligible patients receiving PES. Specifically, patient-facing education and affinity groups can improve patient/caregiver understanding of epilepsy and its treatment, including PES. Additionally, targeting social functioning and identity formation outcomes will address key metrics of patient/caregiver satisfaction with PES. Although there are some in-person epilepsy support groups for patients/caregivers, there remains a need for a social support model that is accessible to traditionally underserved youth with IE.
Methods: We used a community-based participatory research framework to develop a private, moderated, online social community for youth with epilepsy and a corresponding 12-week curriculum focused on identity formation, activities of daily living (ADL), epilepsy self-management, and social skills.
Results: Our pilot cohort (n = 60) includes a subset of 15 (25%) pediatric patients with IE. These IE patients represent a diverse range of demographics: 10 (66.67%) have co-morbid health conditions, 7 (46.67%) use public health insurance, 5 (38.46%) are youth of color, 2 (13.33%) are nonverbal, and 1 (6.67%) requires full support with ADL. Furthermore, our virtual program allowed us to reach patients from 13 different zip codes: 2 (13.33%) in rural communities and all in health professional shortage/medically underserved areas across New England.
Conclusion : The aforementioned cohort demographics indicate that an online, moderated social and educational community for youth with IE is appealing and accessible to traditionally underrepresented PES recipients. These findings suggest that our model can be applied in order to improve social support for a more diverse range of IE patients and, therefore, increase PES utilization among at-risk communities.
Methods: We used a community-based participatory research framework to develop a private, moderated, online social community for youth with epilepsy and a corresponding 12-week curriculum focused on identity formation, activities of daily living (ADL), epilepsy self-management, and social skills.
Results: Our pilot cohort (n = 60) includes a subset of 15 (25%) pediatric patients with IE. These IE patients represent a diverse range of demographics: 10 (66.67%) have co-morbid health conditions, 7 (46.67%) use public health insurance, 5 (38.46%) are youth of color, 2 (13.33%) are nonverbal, and 1 (6.67%) requires full support with ADL. Furthermore, our virtual program allowed us to reach patients from 13 different zip codes: 2 (13.33%) in rural communities and all in health professional shortage/medically underserved areas across New England.
Conclusion : The aforementioned cohort demographics indicate that an online, moderated social and educational community for youth with IE is appealing and accessible to traditionally underrepresented PES recipients. These findings suggest that our model can be applied in order to improve social support for a more diverse range of IE patients and, therefore, increase PES utilization among at-risk communities.
