Angiographic Metrics Alone for Balloon Test Occlusion is a Safe and Effective method to assess Vessel Sacrifice in Pediatric Patients.
Angiographic Metrics Alone for Balloon Test Occlusion Is a Safe and Effective Method to Assess Vessel Sacrifice in Pediatric Patients
Friday, April 21, 2023

Ari Kappel, MD
Resident Physicain
Brigham and Women's Hospital, Dept of Neurosurgery
ePoster Presenter(s)
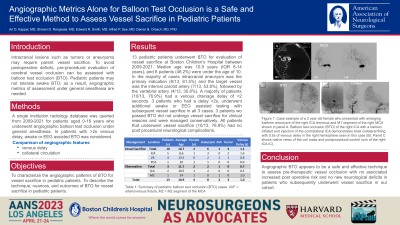
Introduction: Intracranial lesions such as tumors or aneurysms may require parent vessel sacrifice. To avoid postoperative deficits, vessel occlusion can be assessed with balloon test occlusion (BTO). This is done in adults with the assistance of awake neuropsychological testing, however pediatric patients do not tolerate awake BTO. Pediatric BTO can be performed with angiography only metrics of assessment, such as comparison of venous delay between hemispheres, while the patient is under general anesthesia. We report on the single largest series of pediatric BTO performed and associated outcomes.
Methods: A single institution radiology database was queried from 2009-2021 for patients who underwent BTO angiography. All relevant clinical and radiographic data was reviewed.
Results: A total of 17 BTOs were performed at Boston Children’s Hospital from 2009-2021. 13 (76.5%) of these had angiographic – only assessment of vessel occlusion, with the patient under general anesthesia for the procedure. Median age was 13 years old (IQR 8-15 years) and 7 (41.2%) patients were under the age of 10. The leading underlying pathology was associated intracranial aneurysm (8, 47%) followed by tumor (6, 35.2%) and the target vessel was the internal carotid artery (9, 52.9%) in majority of cases, followed by the vertebral artery (6, 35.2%). Majority of patients (11, 84.6%) had a venous drainage delay < 2 seconds. All patients that underwent subsequent vessel sacrifice (10, 72.4%) had no post procedural neurological complications. Only 2 patients had a delay >2 seconds and required additional awake or EEG assisted testing prior to ultimate vessel sacrifice, without any neurological deficits. The sensitivity of angiographic-only BTO was 75% and we were unable to calculate specificity given no events of post operative stroke or deficit after vessel occlusion.
Conclusion : Angiographic BTO alone is a safe and effect technique to assess pre-therapeutic vessel occlusion with no associated increased post operative risk.
Methods: A single institution radiology database was queried from 2009-2021 for patients who underwent BTO angiography. All relevant clinical and radiographic data was reviewed.
Results: A total of 17 BTOs were performed at Boston Children’s Hospital from 2009-2021. 13 (76.5%) of these had angiographic – only assessment of vessel occlusion, with the patient under general anesthesia for the procedure. Median age was 13 years old (IQR 8-15 years) and 7 (41.2%) patients were under the age of 10. The leading underlying pathology was associated intracranial aneurysm (8, 47%) followed by tumor (6, 35.2%) and the target vessel was the internal carotid artery (9, 52.9%) in majority of cases, followed by the vertebral artery (6, 35.2%). Majority of patients (11, 84.6%) had a venous drainage delay < 2 seconds. All patients that underwent subsequent vessel sacrifice (10, 72.4%) had no post procedural neurological complications. Only 2 patients had a delay >2 seconds and required additional awake or EEG assisted testing prior to ultimate vessel sacrifice, without any neurological deficits. The sensitivity of angiographic-only BTO was 75% and we were unable to calculate specificity given no events of post operative stroke or deficit after vessel occlusion.
Conclusion : Angiographic BTO alone is a safe and effect technique to assess pre-therapeutic vessel occlusion with no associated increased post operative risk.
