Deep Brain Stimulation for Treatment of Psychiatric Illness: A Nationally Representative Update
Friday, April 21, 2023

Kavelin Rumalla, MD, MS (he/him/his)
Resident Physician
University of New Mexico
Albuquerque, NM, US
ePoster Presenter(s)
Introduction: The neurosurgical management of medically intractable psychiatric disorders with deep brain stimulation (DBS) is an emerging area of research and clinical practice. To our knowledge, this is the largest analysis of psychiatric DBS procedures (P-DBS) and provides baseline patient characteristics and surgical outcomes that may serve useful for preoperative counseling, surgical decision making, and future research studies.
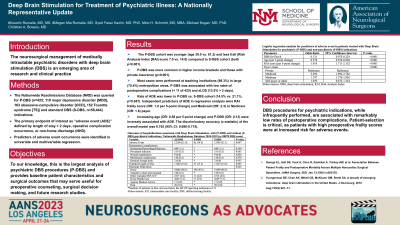
Methods: The Nationwide Readmissions Database (NRD) was queried for P-DBS (n=425; 110 major depressive disorder [MDD], 163 obsessive-compulsive disorder [OCD], 152 Tourette syndrome [TS]) and standard DBS (S-DBS, n=58,444) indications. The primary endpoint of interest as “adverse event (ADE)” defined by length of stay > 2 days, operative complication occurrence, or non-home discharge (NHD). Predictors of adverse event occurrence were identified in univariate and multivariable regression.
Results: The P-DBS cohort was younger (age 39.0 vs. 61.2) and less frail (Risk Analysis Index [RAI] score 7.0 vs. 14.0) compared to S-DBS cohort (both p< 0.001). P-DBS was more commonly in higher income brackets and those with private insurance (p < 0.001). Most cases were performed at teaching institutions (98.3%) in large (70.4%) metropolitan areas. P-DBS was associated with low rates of postoperative complications ( < 11 of 425) and eLOS (13.5% > 2 days). The rate of ADE was lower in P-DBS vs. S-DBS cohort (14.5% vs. 21.1%, p=0.047). Independent predictors of ADE in regression analysis were RAI frailty score (OR: 1.9 per 5-point change) and Medicaid (OR: 2.3) or Medicare (OR: 1.8) payer. Increasing age (OR: 0.58 per 5-point change) and P-DBS (OR: 0.13) were inversely associated with ADE. The discriminatory accuracy (c-statistic) of the overall model was 0.705 (95% CI: 0.696-0.715).
Conclusion : DBS procedures for psychiatric indications, while infrequently performed, are associated with remarkably low rates of postoperative complications. Patient-selection is critical, as patients with high preoperative frailty scores were at increased risk for adverse events.
Methods: The Nationwide Readmissions Database (NRD) was queried for P-DBS (n=425; 110 major depressive disorder [MDD], 163 obsessive-compulsive disorder [OCD], 152 Tourette syndrome [TS]) and standard DBS (S-DBS, n=58,444) indications. The primary endpoint of interest as “adverse event (ADE)” defined by length of stay > 2 days, operative complication occurrence, or non-home discharge (NHD). Predictors of adverse event occurrence were identified in univariate and multivariable regression.
Results: The P-DBS cohort was younger (age 39.0 vs. 61.2) and less frail (Risk Analysis Index [RAI] score 7.0 vs. 14.0) compared to S-DBS cohort (both p< 0.001). P-DBS was more commonly in higher income brackets and those with private insurance (p < 0.001). Most cases were performed at teaching institutions (98.3%) in large (70.4%) metropolitan areas. P-DBS was associated with low rates of postoperative complications ( < 11 of 425) and eLOS (13.5% > 2 days). The rate of ADE was lower in P-DBS vs. S-DBS cohort (14.5% vs. 21.1%, p=0.047). Independent predictors of ADE in regression analysis were RAI frailty score (OR: 1.9 per 5-point change) and Medicaid (OR: 2.3) or Medicare (OR: 1.8) payer. Increasing age (OR: 0.58 per 5-point change) and P-DBS (OR: 0.13) were inversely associated with ADE. The discriminatory accuracy (c-statistic) of the overall model was 0.705 (95% CI: 0.696-0.715).
Conclusion : DBS procedures for psychiatric indications, while infrequently performed, are associated with remarkably low rates of postoperative complications. Patient-selection is critical, as patients with high preoperative frailty scores were at increased risk for adverse events.
