Incidence and Risk Model of Post-Traumatic Hydrocephalus in Patients with Traumatic Brain Injury
Incidence and Risk Model of Post-traumatic Hydrocephalus in Patients with Traumatic Brain Injury
Friday, April 21, 2023

James Pan, MD
Resident Physician
University of Washington
Seattle, Washington, United States
ePoster Presenter(s)
Introduction: Post traumatic hydrocephalus (PTH) is a common complication following traumatic brain injury (TBI) which can delay rehabilitation and lead to morbidity. Early diagnosis and treatment of PTH is essential to improving outcomes and return to function. We report the incidence and risk factors of PTH in a large TBI population while considering death as a competing risk.
Methods: A retrospective cohort study was conducted on consecutive patients with TBI with radiographic intracranial abnormality admitted to our academic medical center from 2005 to 2015. Patient demographics, perioperative data, and in-hospital data were assessed as risk factors for PTH using survival analysis with death as a competing risk.
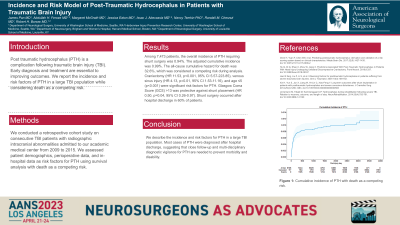
Results: Among 9223 patients, the overall prevalence of PTH requiring shunt surgery was 0.95%. The all-cause mortality rate was 7.7%, which was considered a competing risk during analysis. Craniectomy (HR 14.31 p< 0.001, 95% CI 7.7-26.59), venous sinus injury (HR 2.75, p=0.05, 95% CI 1.02-7.39), intraventricular hemorrhage (HR 1.71, p=0.05, 95% CI 1.00-2.94) and age ≤5 (p < 0.001) were significant risk factors for shunt placement. Glasgow Coma Score (GCS) >13 was protective against shunt placement (p=0.05). After accounting for death as a competing risk, the cumulative incidence for PTH at 10-years post injury is 1.1% and at 8.8 days post injury (mean hospital discharge) is 0.3%.
Conclusion : We describe the incidence and risk factors for PTH in a large TBI population. Most cases of PTH were diagnosed after hospital discharge, which suggests that close follow-up is needed to prevent morbidity and disability.
Methods: A retrospective cohort study was conducted on consecutive patients with TBI with radiographic intracranial abnormality admitted to our academic medical center from 2005 to 2015. Patient demographics, perioperative data, and in-hospital data were assessed as risk factors for PTH using survival analysis with death as a competing risk.
Results: Among 9223 patients, the overall prevalence of PTH requiring shunt surgery was 0.95%. The all-cause mortality rate was 7.7%, which was considered a competing risk during analysis. Craniectomy (HR 14.31 p< 0.001, 95% CI 7.7-26.59), venous sinus injury (HR 2.75, p=0.05, 95% CI 1.02-7.39), intraventricular hemorrhage (HR 1.71, p=0.05, 95% CI 1.00-2.94) and age ≤5 (p < 0.001) were significant risk factors for shunt placement. Glasgow Coma Score (GCS) >13 was protective against shunt placement (p=0.05). After accounting for death as a competing risk, the cumulative incidence for PTH at 10-years post injury is 1.1% and at 8.8 days post injury (mean hospital discharge) is 0.3%.
Conclusion : We describe the incidence and risk factors for PTH in a large TBI population. Most cases of PTH were diagnosed after hospital discharge, which suggests that close follow-up is needed to prevent morbidity and disability.
