Characterization of Sleep in Patients with Parkinson’s Disease
Friday, April 21, 2023

Rig Das, PhD (he/him/his)
Instructor
University of Nebraska Medical Center
Omaha, Nebraska, United States
ePoster Presenter(s)
Introduction: Parkinson’s Disease (PD) patients frequently report poor sleep, which negatively impacts quality of life. However, quantitative data about sleep disturbance is lacking. The objective of this study was to quantify sleep quality in PD patients in a sleep lab setting.
Methods: Three nights of simultaneous polysomnograms (PSG) were obtained in 13 PD subjects (9 Male/4 Female; Age: 53-74), including at least one baseline night and one night with intermittent unilateral subthalamic nucleus (STN) sub-threshold stimulation (30 seconds every 5 minutes; 70% of therapeutic mA) through a percutaneous extension cable connected to a DBS lead. Sleep stage scoring was based on the consensus score determined by four sleep experts. Percentage of time and mean bout length of wake after sleep onset (WASO) and each sleep-stages (NREM stages N1, N2, N3; REM) were calculated and compared between baseline and stimulated nights.
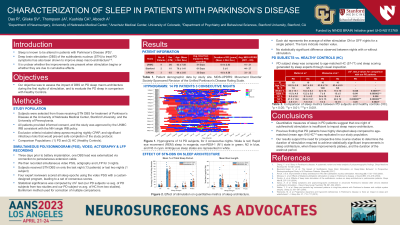
Results: PD patients had highly disrupted sleep on baseline nights with diminished REM and N3. WASO comprised an average (± standard deviation) of [21.6±19.0] % of the sleep period. N2 [84.5±24.2] %, accounted for the majority of sleep, with a small amount of N1 [6.4±3.7] %, N3 [1.4±3.8] %, and REM [7.7±10.3] %. Sleep was also highly fragmented, with mean bout lengths of [1.6±0.7] min for N1, [19.3±13.7] min for N2, [3.7±3.9] min for N3, [6.9±5.5] min for REM, and [9.1±10.2] min for WASO. No statistically significant difference in individual bout length was observed between baseline and stimulated nights.
Conclusion : Objective measures show sleep architecture in PD to be diminished in REM and N3, dominated by N2, highly fragmented, with mean bout lengths less than 10 minutes for all sleep stages except N2. Interestingly, though no objective change in sleep-stage length could be found in response to subthreshold stimulation, the majority of patients reported that stimulation night was their best night of sleep.
Methods: Three nights of simultaneous polysomnograms (PSG) were obtained in 13 PD subjects (9 Male/4 Female; Age: 53-74), including at least one baseline night and one night with intermittent unilateral subthalamic nucleus (STN) sub-threshold stimulation (30 seconds every 5 minutes; 70% of therapeutic mA) through a percutaneous extension cable connected to a DBS lead. Sleep stage scoring was based on the consensus score determined by four sleep experts. Percentage of time and mean bout length of wake after sleep onset (WASO) and each sleep-stages (NREM stages N1, N2, N3; REM) were calculated and compared between baseline and stimulated nights.
Results: PD patients had highly disrupted sleep on baseline nights with diminished REM and N3. WASO comprised an average (± standard deviation) of [21.6±19.0] % of the sleep period. N2 [84.5±24.2] %, accounted for the majority of sleep, with a small amount of N1 [6.4±3.7] %, N3 [1.4±3.8] %, and REM [7.7±10.3] %. Sleep was also highly fragmented, with mean bout lengths of [1.6±0.7] min for N1, [19.3±13.7] min for N2, [3.7±3.9] min for N3, [6.9±5.5] min for REM, and [9.1±10.2] min for WASO. No statistically significant difference in individual bout length was observed between baseline and stimulated nights.
Conclusion : Objective measures show sleep architecture in PD to be diminished in REM and N3, dominated by N2, highly fragmented, with mean bout lengths less than 10 minutes for all sleep stages except N2. Interestingly, though no objective change in sleep-stage length could be found in response to subthreshold stimulation, the majority of patients reported that stimulation night was their best night of sleep.
