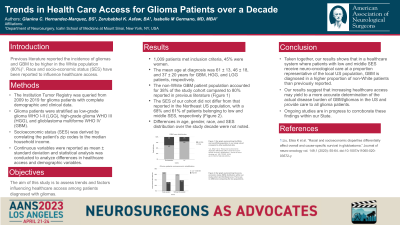
Trends in Health Care Access for Glioma Patients over a Decade
Friday, April 21, 2023
.jpg)
Gianina C. Hernandez-Marquez, BS (she/her/hers)
Medical Student
Icanh School of Medicine at Mount Sinai
San Juan, Puerto Rico, United States
ePoster Presenter(s)
Introduction: Socioeconomic (SE) factors and race impact healthcare access potentially yielding to disparate outcomes. Their toll on gliomas remains overlooked. Yet, the US incidence of gliomas is increasing with over 58,000 new cases predicted in 2022 and a death toll of over 18,000. The aim of this study is to assess trends and factors influencing healthcare access among glioma patients in a large metropolitan medical system.
Methods: Glioma (WHO I-IV) patients with complete demographic and clinical data were identified from the Institution tumor registry (2009-2019) and stratified as low-grade glioma WHO I-II (LGG), high-grade glioma WHO III (HGG), and glioblastoma WHO IV (GBM). The median household income served as a proxy for SE status. The SE distribution of the study cohort was compared with the US Northeast SE population distribution.
Results: 1,009 patients met inclusion criteria, 45% were women. The mean age at diagnosis was 61 ± 13, 46 ± 18, and 37 ± 20 years for GBM, HGG, and LGG patients, respectively, without significant changes over time. The non-white population with GBM was 38% compared to 10% previously reported by others without significant changes over a decade. Based on SE stratification, the overall percentage of middle and low-income glioma patients was similar to the percentage of the US Northeast population, 69% and 61% respectively.
Conclusion : Our study shows that in a healthcare system were low and middle-income patients receive neuro-oncological care at a proportion representative of the local US population with similar SE indicators, GBM is diagnosed in a higher proportion of non-white patients than previously reported. These results suggest that increasing healthcare access may yield to a more accurate account of the actual burden of gliomas in the US and provide care to all glioma patients. Ongoing studies are in progress to corroborate these findings within the State.
Methods: Glioma (WHO I-IV) patients with complete demographic and clinical data were identified from the Institution tumor registry (2009-2019) and stratified as low-grade glioma WHO I-II (LGG), high-grade glioma WHO III (HGG), and glioblastoma WHO IV (GBM). The median household income served as a proxy for SE status. The SE distribution of the study cohort was compared with the US Northeast SE population distribution.
Results: 1,009 patients met inclusion criteria, 45% were women. The mean age at diagnosis was 61 ± 13, 46 ± 18, and 37 ± 20 years for GBM, HGG, and LGG patients, respectively, without significant changes over time. The non-white population with GBM was 38% compared to 10% previously reported by others without significant changes over a decade. Based on SE stratification, the overall percentage of middle and low-income glioma patients was similar to the percentage of the US Northeast population, 69% and 61% respectively.
Conclusion : Our study shows that in a healthcare system were low and middle-income patients receive neuro-oncological care at a proportion representative of the local US population with similar SE indicators, GBM is diagnosed in a higher proportion of non-white patients than previously reported. These results suggest that increasing healthcare access may yield to a more accurate account of the actual burden of gliomas in the US and provide care to all glioma patients. Ongoing studies are in progress to corroborate these findings within the State.
