Cost Associated with Repeat Digital Subtraction Angiogram (DSA) in Initially Angiogram Negative Subarachnoid Hemorrhage Patients
Friday, April 21, 2023
.jpg)
John Bolger
Medical Student
Drexel University College of Medicine
Centerport, New York, United States
ePoster Presenter(s)
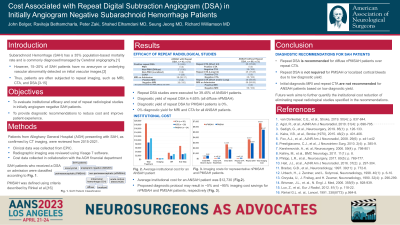
Introduction: Subarachnoid Hemorrhage (SAH) has a 35% population-based mortality rate and is commonly diagnosed and managed by Cerebral angiography.[1] However, 15–20% of SAH patients have no aneurysm or underlying vascular abnormality detected on initial vascular images[2]. Thus, patients are often subjected to repeat imaging, such as MRI, CTA, and DSA.[3-10] Herein, the institutional efficacy and cost of repeat radiological studies in initially angiogram negative SAH patients were evaluated resulting in diagnostic recommendations to reduce cost and improve patient experience.
Methods: Patients from Alleghany General Hospital (AGH) presenting with SAH, as confirmed by CT imaging, were reviewed from 2015-2021. Clinical data was collected from EPIC. Radiographic imaging was reviewed using Visage 7 software. Cost data collected in collaboration with the AGH financial department follows cost accounting methodologies based on allocation of direct costs using relative value units.
Results: SAH patients who received a DSA on admission were classified with aneurysmal or angiogram negative SAH (ANSAH). Repeat DSA studies were executed for 39.45% of ANSAH patients, which was subdivided into perimesencephalic (PMSAH) and non-perimesencephalic (nPMSAH) hemorrhage patterns, including diffuse, localized and cortical SAH. PMSAH was defined using criteria described by Rinkel et al[11]. Repeat DSA was positive in two cases (4.65% positivity rate), both of which presented with diffuse nPMSAH. Notably, short- and long-term repeat CTA and MRI in ANSAH patients produced a 0% diagnostic yield. Average institutional cost for an ANSAH patient was $14,392, which included multiple imaging studies and prolonged ICU stay.
Conclusion : Repeat DSA is recommended for diffuse nPMSAH patients and not required for PMSAH or localized/cortical bleeds due to low diagnostic yield. Repeat CTA and diagnostic MRI are not recommended based on low diagnostic yield. Future work aims to quantify the institutional cost reduction of eliminating repeat radiological studies specified in the recommendations.
Methods: Patients from Alleghany General Hospital (AGH) presenting with SAH, as confirmed by CT imaging, were reviewed from 2015-2021. Clinical data was collected from EPIC. Radiographic imaging was reviewed using Visage 7 software. Cost data collected in collaboration with the AGH financial department follows cost accounting methodologies based on allocation of direct costs using relative value units.
Results: SAH patients who received a DSA on admission were classified with aneurysmal or angiogram negative SAH (ANSAH). Repeat DSA studies were executed for 39.45% of ANSAH patients, which was subdivided into perimesencephalic (PMSAH) and non-perimesencephalic (nPMSAH) hemorrhage patterns, including diffuse, localized and cortical SAH. PMSAH was defined using criteria described by Rinkel et al[11]. Repeat DSA was positive in two cases (4.65% positivity rate), both of which presented with diffuse nPMSAH. Notably, short- and long-term repeat CTA and MRI in ANSAH patients produced a 0% diagnostic yield. Average institutional cost for an ANSAH patient was $14,392, which included multiple imaging studies and prolonged ICU stay.
Conclusion : Repeat DSA is recommended for diffuse nPMSAH patients and not required for PMSAH or localized/cortical bleeds due to low diagnostic yield. Repeat CTA and diagnostic MRI are not recommended based on low diagnostic yield. Future work aims to quantify the institutional cost reduction of eliminating repeat radiological studies specified in the recommendations.
