Impact of Spinal Cord Injury on Pregnancy Outcomes: A Nationwide Analysis
Friday, April 21, 2023

Felicia Sun, MD
Resident
Brown University
Providence, Rhode Island, United States
ePoster Presenter(s)
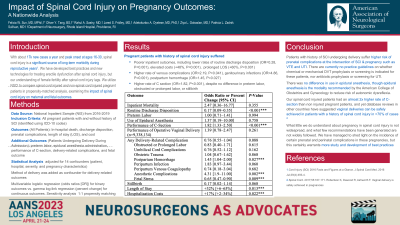
Introduction: Previous case series have indicated that a history of spinal cord injury (SCI) in pregnant patients is associated with higher rates of obstetric complications. However, the general epidemiology of SCI among pregnant patients and nationwide gestational outcomes for this population are poorly understood.
Methods: We identified all pregnant patients with and without history of SCI in the National Inpatient Sample from 2016-2019. For all patients, five outcomes were analyzed: in-hospital death, discharge disposition, prenatal complications, length of stay (LOS), and cost. For patients undergoing delivery during admission, six additional outcomes were studied: preterm labor, epidural anesthesia administration, performance of C-section, delivery-related complications, and fetal outcome. We utilized multivariable logistic and gamma log-link regression to adjust for 14 confounders, including patient, hospital, severity, and pregnancy characteristics.
Results: Among 15,073,815 pregnant admissions from 2016-2019, 1,835 (0.01%) exhibited a history of SCI. 91.6% of admissions were for delivery, with 32.5% undergoing C-sections. Average age was 30.3 years. Among all pregnant admissions, SCI patients had lower rates of routine discharge disposition (odds ratio [OR]=0.28, P=0.001), prolonged LOS (+60%, P=0.001), and elevated costs (+48%, P=0.001). SCI patients exhibited higher odds of prenatal venous complications (OR=2.19, P=0.041) and genitourinary infections (OR=5.02, P=0.001). Moreover, SCI patients were significantly more likely to be admitted non-electively (60.5% vs. 52.1%, P=0.001) and experience non-delivery hospitalizations (OR=2.63, P=0.001). Finally, SCI patients had significantly higher odds of undergoing C-section (OR=1.82, P=0.001). However, among delivery-related admissions, there were no differences in preterm labor, epidural anesthesia administration, delivery-related complications, or stillbirth between SCI and non-SCI patients. All significant associations persisted following 1:1 propensity score matching.
Conclusion : In the first nationwide analysis of pregnancy outcomes among SCI patients, injury history predicted increased rates of nonroutine discharge disposition, LOS, costs, prenatal coagulopathy and infections, non-delivery hospitalizations, and use of C-section, but not stillbirth or delivery-related complications.
Methods: We identified all pregnant patients with and without history of SCI in the National Inpatient Sample from 2016-2019. For all patients, five outcomes were analyzed: in-hospital death, discharge disposition, prenatal complications, length of stay (LOS), and cost. For patients undergoing delivery during admission, six additional outcomes were studied: preterm labor, epidural anesthesia administration, performance of C-section, delivery-related complications, and fetal outcome. We utilized multivariable logistic and gamma log-link regression to adjust for 14 confounders, including patient, hospital, severity, and pregnancy characteristics.
Results: Among 15,073,815 pregnant admissions from 2016-2019, 1,835 (0.01%) exhibited a history of SCI. 91.6% of admissions were for delivery, with 32.5% undergoing C-sections. Average age was 30.3 years. Among all pregnant admissions, SCI patients had lower rates of routine discharge disposition (odds ratio [OR]=0.28, P=0.001), prolonged LOS (+60%, P=0.001), and elevated costs (+48%, P=0.001). SCI patients exhibited higher odds of prenatal venous complications (OR=2.19, P=0.041) and genitourinary infections (OR=5.02, P=0.001). Moreover, SCI patients were significantly more likely to be admitted non-electively (60.5% vs. 52.1%, P=0.001) and experience non-delivery hospitalizations (OR=2.63, P=0.001). Finally, SCI patients had significantly higher odds of undergoing C-section (OR=1.82, P=0.001). However, among delivery-related admissions, there were no differences in preterm labor, epidural anesthesia administration, delivery-related complications, or stillbirth between SCI and non-SCI patients. All significant associations persisted following 1:1 propensity score matching.
Conclusion : In the first nationwide analysis of pregnancy outcomes among SCI patients, injury history predicted increased rates of nonroutine discharge disposition, LOS, costs, prenatal coagulopathy and infections, non-delivery hospitalizations, and use of C-section, but not stillbirth or delivery-related complications.
