Clinical Characteristics and Risk Factors of Revision Surgery in Adult Degenerative Scoliosis
Friday, April 21, 2023

Soummitra Anand (she/her/hers)
Medical Student
UT Southwestern Medical Center
Dallas, Texas, United States
ePoster Presenter(s)
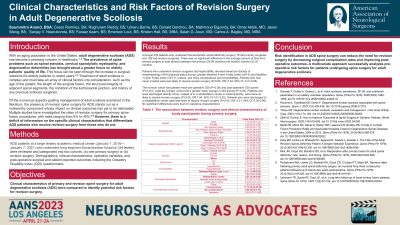
Introduction: We hoped to assess differences in complication rates and patient-reported outcomes between patients undergoing a singular, primary adult degenerative scoliosis (ADS) spine surgery versus those who have had revision surgery for ADS.
Methods: 235 patients who underwent thoracolumbar spinal deformity surgery (≥ 4 levels) were identified and categorized into two cohorts based on whether they had either one primary (N=76) or multiple/revision (N=159) surgeries. Demographics, clinical characteristics, peri-operative variables, and post-operative surgical and patient-reported outcomes were analyzed. The Student’s t, Pearson’s chi-squared, and two-proportion Z tests were performed for statistical analyses, and significance was set to p< 0.05.
Results: Patients in the revision surgery cohort were more likely to have higher BMIs and complication rates and more comorbidities. Patients with BMIs in the normal range were less likely to require revision surgery. Similarly, those who had never smoked were less likely to require revision surgery. On average, pre-operative INR was lower for the revision cohort. The revision cohort had greater mean pre-operative ODI, post-operative ODI, mFI-5, and mFI-11 scores while the primary cohort had a greater mean change in ODI scores. Patients who were discharged directly home instead of a rehabilitation center or medical facility were almost two times more likely to require revision surgery. In contrast, patients who were discharged to the Zale Lipshy Pavilion Rehabilitation Center were less likely to require revision surgery.
Conclusion : The purpose of spinal fusion surgery is not only to restore structure and function to patients but to prevent further damage and complications and reduce disease morbidity. Therefore, an individualistic and multivariate approach must be taken when assessing pre-operative risk factors for patients undergoing spine surgery for ADS. Identifying such risk factors and altering surgical management accordingly could minimize the need for revision surgeries, decrease financial burden, and improve patient outcomes.
Methods: 235 patients who underwent thoracolumbar spinal deformity surgery (≥ 4 levels) were identified and categorized into two cohorts based on whether they had either one primary (N=76) or multiple/revision (N=159) surgeries. Demographics, clinical characteristics, peri-operative variables, and post-operative surgical and patient-reported outcomes were analyzed. The Student’s t, Pearson’s chi-squared, and two-proportion Z tests were performed for statistical analyses, and significance was set to p< 0.05.
Results: Patients in the revision surgery cohort were more likely to have higher BMIs and complication rates and more comorbidities. Patients with BMIs in the normal range were less likely to require revision surgery. Similarly, those who had never smoked were less likely to require revision surgery. On average, pre-operative INR was lower for the revision cohort. The revision cohort had greater mean pre-operative ODI, post-operative ODI, mFI-5, and mFI-11 scores while the primary cohort had a greater mean change in ODI scores. Patients who were discharged directly home instead of a rehabilitation center or medical facility were almost two times more likely to require revision surgery. In contrast, patients who were discharged to the Zale Lipshy Pavilion Rehabilitation Center were less likely to require revision surgery.
Conclusion : The purpose of spinal fusion surgery is not only to restore structure and function to patients but to prevent further damage and complications and reduce disease morbidity. Therefore, an individualistic and multivariate approach must be taken when assessing pre-operative risk factors for patients undergoing spine surgery for ADS. Identifying such risk factors and altering surgical management accordingly could minimize the need for revision surgeries, decrease financial burden, and improve patient outcomes.
