Intrathecal devices for monitoring of the spinal cord cord perfussion pressure: systematic review
Intrathecal Devices for Monitoring of the Spinal Cord Cord Perfussion Pressure: Systematic Review
Friday, April 21, 2023

Samuel N. Brehm, BSME (he/him/his)
Medical Student
Washington University School of Medicine
Corpus Christi, Texas, United States
ePoster Presenter(s)
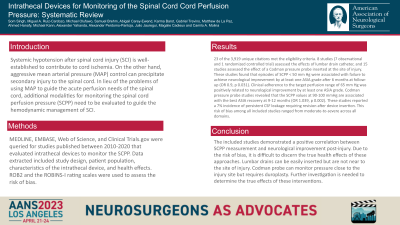
Introduction: It is well-known that systemic hypotension after spinal cord injury (SCI) contributes to cord ischemia, but also aggressive mean arterial pressure (MAP) management can favor secondary injury to the spinal cord. In lieu of the problems of using MAP to guide the acute perfusion needs of the spinal cord, methods for monitoring the spinal cord perfusion pressure (SCPP) to guide hemodynamic management of SCI in the setting of SCI. The objective of this study was to identify the health effects of using different invasive intrathecal devices.
Methods: An electronic search was conducted for studies that evaluated intrathecal devices to monitor the spinal cord perfusion. Two reviewers independently screened articles, extracted data. The ROB2 and the ROBINS-I rating scales were used to assess the risk of bias of the reported health effects.
Results: We obtained 3,919 unique citations, 23 of which met the eligibility criteria. 8 studies evaluated the effects of lumbar drain catheter. These studies found that episodes of SCPP < 50mm Hg were associated with failure to achieve neurological improvement by at least one AIS grade after 6 months at follow-up. These studies did not reported any major adverse events. 15 studies assessed the effect of a Codman pressure probe inserted at the site of injury. These studies informed that the SCPP values at 90-100mmHg are associated with the best ASIA recovery at 9-12 months. These studies reported a 7% incidence of persistent CSF leakage requiring revision after device insertion. The risk of bias among all included studies ranged from the moderate-to-serious across all domains.
Conclusion : We found two approaches to measure the spinal cord perfusion pressure: via lumbar catheter drains and Codman pressure probes inserted at the site of injury. Due to the moderate to high risk of bias of the studies, it is difficult to ascertain their true health effects.
Methods: An electronic search was conducted for studies that evaluated intrathecal devices to monitor the spinal cord perfusion. Two reviewers independently screened articles, extracted data. The ROB2 and the ROBINS-I rating scales were used to assess the risk of bias of the reported health effects.
Results: We obtained 3,919 unique citations, 23 of which met the eligibility criteria. 8 studies evaluated the effects of lumbar drain catheter. These studies found that episodes of SCPP < 50mm Hg were associated with failure to achieve neurological improvement by at least one AIS grade after 6 months at follow-up. These studies did not reported any major adverse events. 15 studies assessed the effect of a Codman pressure probe inserted at the site of injury. These studies informed that the SCPP values at 90-100mmHg are associated with the best ASIA recovery at 9-12 months. These studies reported a 7% incidence of persistent CSF leakage requiring revision after device insertion. The risk of bias among all included studies ranged from the moderate-to-serious across all domains.
Conclusion : We found two approaches to measure the spinal cord perfusion pressure: via lumbar catheter drains and Codman pressure probes inserted at the site of injury. Due to the moderate to high risk of bias of the studies, it is difficult to ascertain their true health effects.
