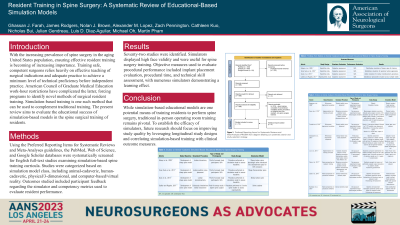
Resident Training in Spine Surgery: The Current Landscape of Simulation-Based Educational Models
Resident Training in Spine Surgery: The Current Landscape of Simulation-based Educational Models
Friday, April 21, 2023
Nolan J. Brown, MBA
Junior Specialist
UC Irvine Department of Neurosurgery
Santa Clarita, California, United States
ePoster Presenter(s)
Introduction: Spine surgery makes a large portion of most neurosurgery practices and training the next generation of spine surgeons is crucial. This relies heavily on effective teaching so that optimal patient outcomes are obtained. With the restriction on neurosurgery resident work hours formulated by the American Council of Graduate Medical Education (ACGME), institutions have sought novel methods of surgical resident training. One example is simulation-based training, a valuable complement to traditional training in the operating room. Given the increased relevance of this training modality in recents years, this review aims to determine the educational success of simulation-based models in the spine surgical training of residents.
Methods: After systematically querying and screening papers from PubMed, Web of Science, and Google Scholar, 72 studies were relevant and categorized based on simulation model class, including animal-cadaveric, human-cadaveric, physical/three-dimensional, and computer-based/virtual reality. Outcomes studied included participant feedback regarding the simulator and competency metrics used to evaluate participant performance.
Results: Simulators displayed high face validity and were useful for spine surgery training. Objective measures used to evaluate procedural performance included implant placement evaluation, procedural time, and technical skill assessment, with numerous simulators demonstrating a learning effect. Limitations in the current literature regarding simulator use in spine surgery resident training include the small sample sizes of residents considered, flawed study designs, and lack of correlation with both operating room performance and salient patient outcomes.
Conclusion : While simulation-based educational models are one potential means of training residents to perform spine surgery, traditional in-person operating room training remains pivotal. To establish the efficacy of simulators, future research should focus on improving study quality by leveraging longitudinal study designs and correlating simulation-based training with clinical outcome measures.
Methods: After systematically querying and screening papers from PubMed, Web of Science, and Google Scholar, 72 studies were relevant and categorized based on simulation model class, including animal-cadaveric, human-cadaveric, physical/three-dimensional, and computer-based/virtual reality. Outcomes studied included participant feedback regarding the simulator and competency metrics used to evaluate participant performance.
Results: Simulators displayed high face validity and were useful for spine surgery training. Objective measures used to evaluate procedural performance included implant placement evaluation, procedural time, and technical skill assessment, with numerous simulators demonstrating a learning effect. Limitations in the current literature regarding simulator use in spine surgery resident training include the small sample sizes of residents considered, flawed study designs, and lack of correlation with both operating room performance and salient patient outcomes.
Conclusion : While simulation-based educational models are one potential means of training residents to perform spine surgery, traditional in-person operating room training remains pivotal. To establish the efficacy of simulators, future research should focus on improving study quality by leveraging longitudinal study designs and correlating simulation-based training with clinical outcome measures.
