Characterizing and Improving Nomenclature for Reporting Lumbar Interbody Fusion Techniques
Friday, April 21, 2023

Hasan S. Ahmad, BS
Medical Student
University of Pennsylvania
Philadelphia, Pennsylvania, United States
ePoster Presenter(s)
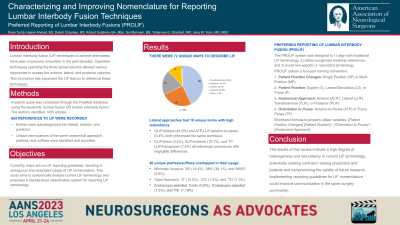
Introduction: Lumbar interbody fusion (LIF) techniques have seen impressive innovation in the past decades. This innovation has expanded the LIF lexicon to reference these techniques. Currently, there are no LIF reporting guidelines, resulting in ambiguous and redundant usage of LIF nomenclature. This study aims to systemically analyze current LIF terminology to develop a foundation for creating LIF nomenclature guidelines to improve communication in the spine surgery community.
Methods: A search query was conducted through the PubMed database using the keywords “lumbar fusion OR lumbar interbody fusion.” The authors identified 1455 articles. Following review, 605 references to LIF were recorded. LIF entries were then subcategorized for further analysis according to the anatomical approach to the spine (anterior, lateral, posterior, and transforaminal). Unique permutations of the same anatomical approach, prefixes, and suffixes were identified and recorded.
Results: The most referenced anatomical approaches were transforaminal (43.0%), followed by posterior (25.0%), lateral (19.7%), and anterior (10.9%). Overall, there were 72 unique ways to describe LIF. Lateral approaches had 18 unique terms with a high degree of redundancy. OLIF/oblique (44.5%) and ATP-LLIF/anterior-to-psoas (3.4%) both referenced the same technique, and DLIF/direct (3.4%), XLIF/extreme (15.1%), and TP-LLIF/transpsoas (7.6%) all referenced procedures with negligible differences. Unique prefixes were recorded by approach (posterior: 26; lateral: 13; anterior: 3). 40 unique prefixes/suffixes overlapped in their usage. ‘MI’ (14.4%), ‘MIS’ (38.1%), and ’MISS’ (0.6%) all referenced a minimally invasive approach. ‘O’ (12.5%), ‘CO’ (1.3%), and ‘TO’ (1.3%) all described open techniques. ‘Endo’ (0.6%), ‘Endoscopic-assisted’ (1.3%), and ‘PE’ (1.9%) all referenced endoscopic-assisted procedures.
Conclusion : The results of this review indicate a high degree of heterogeneity and redundancy in current LIF terminology, potentially creating confusion among physicians and patients and compromising the validity of future research. Implementing reporting guidelines for LIF nomenclature could improve communication in the spine surgery community.
Methods: A search query was conducted through the PubMed database using the keywords “lumbar fusion OR lumbar interbody fusion.” The authors identified 1455 articles. Following review, 605 references to LIF were recorded. LIF entries were then subcategorized for further analysis according to the anatomical approach to the spine (anterior, lateral, posterior, and transforaminal). Unique permutations of the same anatomical approach, prefixes, and suffixes were identified and recorded.
Results: The most referenced anatomical approaches were transforaminal (43.0%), followed by posterior (25.0%), lateral (19.7%), and anterior (10.9%). Overall, there were 72 unique ways to describe LIF. Lateral approaches had 18 unique terms with a high degree of redundancy. OLIF/oblique (44.5%) and ATP-LLIF/anterior-to-psoas (3.4%) both referenced the same technique, and DLIF/direct (3.4%), XLIF/extreme (15.1%), and TP-LLIF/transpsoas (7.6%) all referenced procedures with negligible differences. Unique prefixes were recorded by approach (posterior: 26; lateral: 13; anterior: 3). 40 unique prefixes/suffixes overlapped in their usage. ‘MI’ (14.4%), ‘MIS’ (38.1%), and ’MISS’ (0.6%) all referenced a minimally invasive approach. ‘O’ (12.5%), ‘CO’ (1.3%), and ‘TO’ (1.3%) all described open techniques. ‘Endo’ (0.6%), ‘Endoscopic-assisted’ (1.3%), and ‘PE’ (1.9%) all referenced endoscopic-assisted procedures.
Conclusion : The results of this review indicate a high degree of heterogeneity and redundancy in current LIF terminology, potentially creating confusion among physicians and patients and compromising the validity of future research. Implementing reporting guidelines for LIF nomenclature could improve communication in the spine surgery community.
