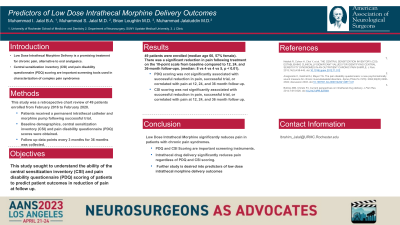
Predictors of Low Dose Intrathecal Morphine Delivery Outcomes
Friday, April 21, 2023
Muhammad I. Jalal (he/him/his)
Medical Student
University of Rochester School of Medicine
Rochester, New York, United States
ePoster Presenter(s)
Introduction: The use of low-dose intrathecal morphine via a morphine drug delivery system is a promising long-term treatment solution for chronic pain and an alternative to oral analgesics. However, little research has been done on other baseline factors that may predicate outcomes for patients receiving this treatment. This study sought to understand the ability of the central sensitization inventory (CSI) and pain disability questionnaire (PDQ) scoring of patients to predicate patient outcomes.
Methods: This was a retrospective chart review of 49 patients. Patients were enrolled from February 2016 to February 2020. Following at least a 60% reduction in pain on an outpatient trial, a permanent intrathecal catheter and morphine pump was implanted. Data were collected starting at 3 months prior to implantation, and every 3 months for 36 months post-implantation.
Results: 49 patients were enrolled (median age 60, 57% female). There was a significant reduction in pain following treatment on the 10-point scale from baseline compared to 12, 24, and 36-month follow-ups. (median: 8 vs 4 vs 4 vs 5, p < 0.01). Interestingly, PDQ and CSI scoring was not found to correlate well with baseline, 12-month, 24-month, and 36-month pain scores or intrathecal drug delivery dosing. There were no infections or complications present in the study.
Conclusion : Low-dose intrathecal drug delivery was shown to significantly reduce pain following treatment. PDQ and CSI scoring was not found to be a good predictor of intrathecal morphine delivery outcomes. This study further characterizes the efficacy of low-dose intrathecal drug delivery, but no standardized inventory exists with good predictability of intrathecal morphine delivery outcomes. Pre-implant pain scores and successful trials may be the best predictors of outcome.
Methods: This was a retrospective chart review of 49 patients. Patients were enrolled from February 2016 to February 2020. Following at least a 60% reduction in pain on an outpatient trial, a permanent intrathecal catheter and morphine pump was implanted. Data were collected starting at 3 months prior to implantation, and every 3 months for 36 months post-implantation.
Results: 49 patients were enrolled (median age 60, 57% female). There was a significant reduction in pain following treatment on the 10-point scale from baseline compared to 12, 24, and 36-month follow-ups. (median: 8 vs 4 vs 4 vs 5, p < 0.01). Interestingly, PDQ and CSI scoring was not found to correlate well with baseline, 12-month, 24-month, and 36-month pain scores or intrathecal drug delivery dosing. There were no infections or complications present in the study.
Conclusion : Low-dose intrathecal drug delivery was shown to significantly reduce pain following treatment. PDQ and CSI scoring was not found to be a good predictor of intrathecal morphine delivery outcomes. This study further characterizes the efficacy of low-dose intrathecal drug delivery, but no standardized inventory exists with good predictability of intrathecal morphine delivery outcomes. Pre-implant pain scores and successful trials may be the best predictors of outcome.
