Insurance Centered Disparities in Surgical Management of Traumatic Brain Injury: a Retrospective Study
Insurance Centered Disparities in Surgical Management of Traumatic Brain Injury: A Retrospective Study
Friday, April 21, 2023

Anthony M. DiGiorgio, DO, MHA
Assistant Professor
University of California San Francisco
San Francisco, California, United States
ePoster Presenter(s)
Introduction: Surgical interventions are often utilized in the acute stage of care for patients with traumatic brain injury (TBI). Adherence to clinical guidelines outlining the use of these interventions is instrumental in successful TBI management and outcomes. However, racial, and socioeconomic factors have been shown to be associated with disparities in other aspects of TBI care. Here we investigate the effects of insurance type on disparities in surgical management of TBI.
Methods: The 2014-2016 National Trauma Data Bank (NTDB) Research Data Set was used for a retrospective cohort study. Patients with Medicaid insurance were compared to private insurance (Medicare was excluded to eliminate the age bias). A patient was categorized as undergoing a TBI interventional procedure (IP) if they had a surgery or Intracranial pressure monitor (ICP) placed. Disparities in TBI management were compared and adjusted for TBI severity utilizing Glasgow Coma Scale (GCS). Data was adjusted for frailty using the modified 5-item frailty index. Linear and logistic regression analysis was performed using insurance type as dependent variable on TBI management.
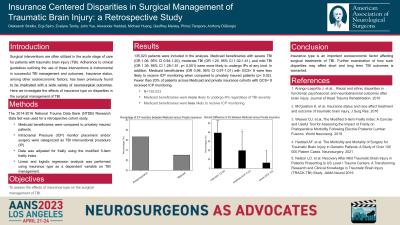
Results: 135,023 patients were included in the analysis. When adjusted for frailty, Medicaid beneficiaries with severe TBI (OR 1.06, 95% CI 0.94-1.20), moderate TBI (OR 1.20, 95% CI 1.02-1.41), and mild TBI (OR 1.39, 95% CI 1.28-1.51, p< 0.001) were more likely to undergo IPs of any kind. In addition, Medicaid beneficiaries (OR 0.98, 95% CI 0.97-1.01) with GCS < 8 were less likely to receive ICP monitoring when compared to privately insured patients (p < 0.02). Fewer than 20% of patients across Medicaid and private insurance cohorts with GCS < 8 received ICP monitoring.
Conclusion : Insurance type is an important socioeconomic factor affecting surgical treatments of TBI. Further examination of how such disparities may affect short and long term TBI outcomes is warranted.
Methods: The 2014-2016 National Trauma Data Bank (NTDB) Research Data Set was used for a retrospective cohort study. Patients with Medicaid insurance were compared to private insurance (Medicare was excluded to eliminate the age bias). A patient was categorized as undergoing a TBI interventional procedure (IP) if they had a surgery or Intracranial pressure monitor (ICP) placed. Disparities in TBI management were compared and adjusted for TBI severity utilizing Glasgow Coma Scale (GCS). Data was adjusted for frailty using the modified 5-item frailty index. Linear and logistic regression analysis was performed using insurance type as dependent variable on TBI management.
Results: 135,023 patients were included in the analysis. When adjusted for frailty, Medicaid beneficiaries with severe TBI (OR 1.06, 95% CI 0.94-1.20), moderate TBI (OR 1.20, 95% CI 1.02-1.41), and mild TBI (OR 1.39, 95% CI 1.28-1.51, p< 0.001) were more likely to undergo IPs of any kind. In addition, Medicaid beneficiaries (OR 0.98, 95% CI 0.97-1.01) with GCS < 8 were less likely to receive ICP monitoring when compared to privately insured patients (p < 0.02). Fewer than 20% of patients across Medicaid and private insurance cohorts with GCS < 8 received ICP monitoring.
Conclusion : Insurance type is an important socioeconomic factor affecting surgical treatments of TBI. Further examination of how such disparities may affect short and long term TBI outcomes is warranted.
