Utilizing Discharge Summary Readability to Predict Outcomes in Cranioplasty Patients
Friday, April 21, 2023

Muhammad S. Ghauri, MS (he/him/his)
Medical Student
California University of Science and Medicine
Rancho Cucamonga, California, United States
ePoster Presenter(s)
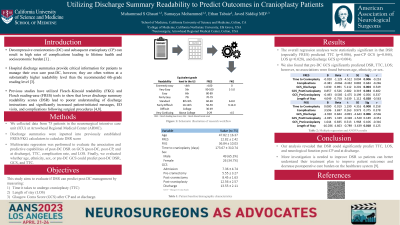
Introduction: Decompressive craniectomies (DC) and subsequent cranioplasty (CP) are common procedures in traumatic brain injury (TBI) management that can result in high rates of complications leading to lifetime health and socioeconomic burden [1]. Hospital discharge summaries provide critical information for patients to manage their own care post-DC, however, they are often written at a substantially higher readability level than recommended (ie, 6th-grade level) [2-3]. Previous studies have utilized Flesch–Kincaid readability (FKG) and Flesch reading-ease (FRES) tools to show that lower discharge readability scores (DSR) lead to poorer understanding of discharge instructions and significantly increased patient-initiated messages, ED visits, and complications following surgical procedures [4,8]. This paper aims to evaluate if DSR can predict post-DC management, specifically the time it takes to undergo cranioplasty (TTC), length of stay (LOS), and Glasgow Coma Score (GCS) after CP and at discharge.
Methods: We collected data from 76 patients in the neurosurgical intensive care unit (ICU) at Arrowhead Regional Medical Center (ARMC). Multivariate regression was performed to evaluate the association and predictive capabilities of post-DC DSR on GCS (post-DC, post-CP, and at discharge), TTC, complication rate, and LOS. Finally, we evaluated whether age, ethnicity, sex, or pre-DC GCS could predict post-DC DSR, GCS, and TTC.
Results: The overall regression analyses were statistically significant in that DSR predicted post-CP GCS (r=0.482, p=0.0.014), TTC (r=0.37, p=0.017), LOS (r=.563, p=0.028), and discharge GCS (r=0.549, p=0.032). We also found that pre-DC GCS significantly predicted DSR, TTC, LOS; however, no associations were found between age, ethnicity, or sex.
Conclusion : Our analysis revealed that DSR could significantly predict TTC, LOS, and neurological function post-CP and at discharge. More investigation is needed to improve DSR so patients can better understand their treatment plan to improve patient outcomes and decrease postoperative care burden on the healthcare system [9].
Methods: We collected data from 76 patients in the neurosurgical intensive care unit (ICU) at Arrowhead Regional Medical Center (ARMC). Multivariate regression was performed to evaluate the association and predictive capabilities of post-DC DSR on GCS (post-DC, post-CP, and at discharge), TTC, complication rate, and LOS. Finally, we evaluated whether age, ethnicity, sex, or pre-DC GCS could predict post-DC DSR, GCS, and TTC.
Results: The overall regression analyses were statistically significant in that DSR predicted post-CP GCS (r=0.482, p=0.0.014), TTC (r=0.37, p=0.017), LOS (r=.563, p=0.028), and discharge GCS (r=0.549, p=0.032). We also found that pre-DC GCS significantly predicted DSR, TTC, LOS; however, no associations were found between age, ethnicity, or sex.
Conclusion : Our analysis revealed that DSR could significantly predict TTC, LOS, and neurological function post-CP and at discharge. More investigation is needed to improve DSR so patients can better understand their treatment plan to improve patient outcomes and decrease postoperative care burden on the healthcare system [9].
