Outcomes After Laminoplasty in Rheumatoid Arthritis Patients With Cervical Spondylotic Myelopathy
Outcomes After Laminoplasty in Rheumatoid Arthritis Patients with Cervical Spondylotic Myelopathy
Friday, April 21, 2023

John J. Francis, BS (he/him/his)
Medical Student
Case Western Reserve University School of Medicine
Cleveland, Ohio, United States
ePoster Presenter(s)
Introduction: Cervical laminoplasty has emerged as a promising surgical intervention for cervical spondylotic myelopathy in patients with rheumatoid arthritis (RA). However, whether RA patients experience adverse clinical outcomes due to underlying RA pathophysiology and various medication use is understudied. We sought to assess the clinical and radiographic outcomes of RA patients following cervical laminoplasty in comparison to non-RA patients.
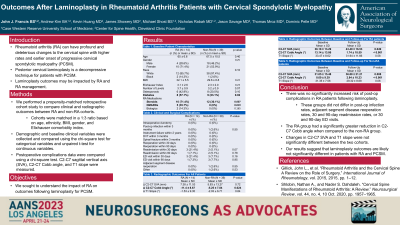
Methods: The RA and non-RA cohorts were propensity-score matched in a 1:3 ratio. Demographic and baseline clinical variables were collected and compared using the chi-square test for categorical variables and unpaired t-test for continuous variables. Postoperative complications data was compared using a Pearson chi-square test. A paired t-test was used to evaluate the pre- to post-operative change in radiographic metrics within each cohort and unpaired t-tests were used to compare the values between the RA and non-RA cohorts.
Results: After exclusion of hybrid procedures and inadequate imaging, a total of 53 patients (RA: 14; non-RA: 39) were included. The average age was 66.86 ± 9.67 years, and 41.5% of patients were male. RA and non-RA groups did not differ in post-operative infection rates (p = 0.545), adjacent segment disease re-operation rates (p = 0.545), 30 and 90-day readmission (p = 0.073, p = 0.78), or 30 and 90-day ED visit (p = 0.164, p = 0.947). The RA group had a significantly greater reduction in C2-C7 Cobb angle compared to the non-RA group (p = 0.024). However, changes in C2-C7 sagittal vertical axis (p = 0.717) and T1 slope (p = 0.835) were not significantly different between the two cohorts.
Conclusion : Surgical and medical complication rates are non-significant between the RA and non-RA patient cohorts. There was no significantly increased risk of complications in RA patients following laminoplasty relative to their non-RA counterparts.
Methods: The RA and non-RA cohorts were propensity-score matched in a 1:3 ratio. Demographic and baseline clinical variables were collected and compared using the chi-square test for categorical variables and unpaired t-test for continuous variables. Postoperative complications data was compared using a Pearson chi-square test. A paired t-test was used to evaluate the pre- to post-operative change in radiographic metrics within each cohort and unpaired t-tests were used to compare the values between the RA and non-RA cohorts.
Results: After exclusion of hybrid procedures and inadequate imaging, a total of 53 patients (RA: 14; non-RA: 39) were included. The average age was 66.86 ± 9.67 years, and 41.5% of patients were male. RA and non-RA groups did not differ in post-operative infection rates (p = 0.545), adjacent segment disease re-operation rates (p = 0.545), 30 and 90-day readmission (p = 0.073, p = 0.78), or 30 and 90-day ED visit (p = 0.164, p = 0.947). The RA group had a significantly greater reduction in C2-C7 Cobb angle compared to the non-RA group (p = 0.024). However, changes in C2-C7 sagittal vertical axis (p = 0.717) and T1 slope (p = 0.835) were not significantly different between the two cohorts.
Conclusion : Surgical and medical complication rates are non-significant between the RA and non-RA patient cohorts. There was no significantly increased risk of complications in RA patients following laminoplasty relative to their non-RA counterparts.
