Factors predicting cerebrospinal fluid leaks in microvascular decompressions
Factors Predicting Cerebrospinal Fluid Leaks in Microvascular Decompressions
Friday, April 21, 2023

Raymond J. So, AB (he/him/his)
Medical Student
Johns Hopkins University School of Medicine
ePoster Presenter(s)
Introduction: Microvascular decompression (MVD) via a retrosigmoid approach is a highly effective, open-surgical procedure for neurovascular conflict in the posterior fossa, although there is a risk of postoperative cerebrospinal fluid (CSF) leak. Factors associated with postoperative CSF leakage following MVD are incompletely characterized in the literature.
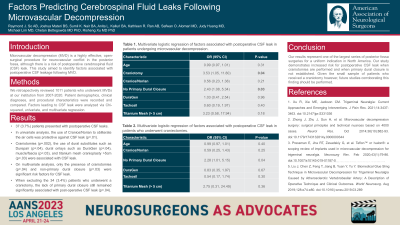
Methods: We retrospectively reviewed all patients who underwent MVDs at our institution from 2007-2020. Patient demographics, clinical diagnoses, and procedural characteristics were recorded and compared between patients with and without postoperative CSF leakage. Differences in categorical variables were analyzed using chi-squared analyses, while differences in continuous variables were assessed using a t-test. Significant characteristics were then analyzed using a univariate logistic regression. Significant variables from univariate regressions were then analyzed using a multivariate logistic regression.
Results: Out of 1011 patients who underwent MVDs, 37 (3.7%) presented with postoperative CSF leaks. In univariate analysis, the use of Cranios/Norian to obliterate the air cells was protective against CSF leak (p=.01). Craniotomies (p=.002), the use of dural substitutes such as Durepair (p=.04), dural onlays such as DuraGen (p=.04), muscle/fascia (p=.03), and titanium mesh cranioplasty >5cm (p=.03) were associated with CSF leak. On multivariate analysis, only the presence of craniotomies (p=.04) and non-primary dural closure (p=.03) were significant risk factors for CSF leak. When excluding the 34 (3.4%) patients who underwent a craniotomy, the lack of primary dural closure remained significantly associated with post-operative CSF leak (p=.04).
Conclusion : Our results represent one of the largest series of posterior fossa surgeries for a uniform indication in North America. Our study demonstrates increased risk for postoperative CSF leak when craniotomies are performed and when primary dural closure is not established. Given the small sample of patients who received a craniotomy, future studies corroborating this finding should be performed.
Methods: We retrospectively reviewed all patients who underwent MVDs at our institution from 2007-2020. Patient demographics, clinical diagnoses, and procedural characteristics were recorded and compared between patients with and without postoperative CSF leakage. Differences in categorical variables were analyzed using chi-squared analyses, while differences in continuous variables were assessed using a t-test. Significant characteristics were then analyzed using a univariate logistic regression. Significant variables from univariate regressions were then analyzed using a multivariate logistic regression.
Results: Out of 1011 patients who underwent MVDs, 37 (3.7%) presented with postoperative CSF leaks. In univariate analysis, the use of Cranios/Norian to obliterate the air cells was protective against CSF leak (p=.01). Craniotomies (p=.002), the use of dural substitutes such as Durepair (p=.04), dural onlays such as DuraGen (p=.04), muscle/fascia (p=.03), and titanium mesh cranioplasty >5cm (p=.03) were associated with CSF leak. On multivariate analysis, only the presence of craniotomies (p=.04) and non-primary dural closure (p=.03) were significant risk factors for CSF leak. When excluding the 34 (3.4%) patients who underwent a craniotomy, the lack of primary dural closure remained significantly associated with post-operative CSF leak (p=.04).
Conclusion : Our results represent one of the largest series of posterior fossa surgeries for a uniform indication in North America. Our study demonstrates increased risk for postoperative CSF leak when craniotomies are performed and when primary dural closure is not established. Given the small sample of patients who received a craniotomy, future studies corroborating this finding should be performed.
