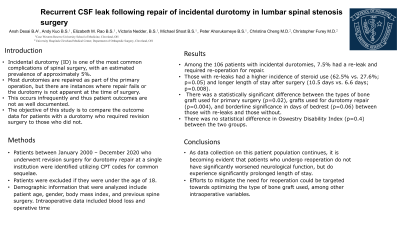
Recurrent CSF leak following repair of incidental durotomy in lumbar spinal stenosis surgery
Recurrent CSF Leak Following Repair of Incidental Durotomy in Lumbar Spinal Stenosis Surgery
Friday, April 21, 2023
Ansh D. Desai
Medical Student
Case Western Reserve University School of Medicine
Cleveland, Ohio, United States
ePoster Presenter(s)
Introduction: Incidental durotomy (ID) is one of the most common complications of spinal surgery, with an estimated prevalence of approximately 5%. Most durotomies are repaired as part of the primary operation, but there are instances where repair fails or the durotomy is not apparent at the time of surgery. This occurs infrequently and thus patient outcomes are not as well documented. Therefore, the objective of this study is to compare the outcome data for patients with a durotomy who required revision surgery to those who did not.
Methods: Patients between January 2000 – December 2020 who underwent revision surgery for durotomy repair at a single institution were identified utilizing CPT codes for common sequelae. Patients were excluded if they were under the age of 18. Demographic information that were analyzed include patient age, gender, body mass index, and previous spine surgery. Intraoperative data included blood loss and operative time.
Results: Among the 106 patients with incidental durotomies, 7.5% had a re-leak and required re-operation for repair. Those with re-leaks had a higher incidence of steroid use (62.5% vs. 27.6%; p=0.05) and longer length of stay after surgery (10.5 days vs. 6.6 days; p=0.008). There was a statistically significant difference between the types of bone graft used for primary surgery (p=0.02), grafts used for durotomy repair (p=0.004), and borderline significance in days of bedrest (p=0.06) between those with re-leaks and those without. There was no statistical difference in Oswestry Disability Index (p=0.4) between the two groups.
Conclusion : As data collection on this patient population continues, it is becoming evident that patients who undergo reoperation do not have significantly worsened neurological function, but do experience significantly prolonged length of stay. Therefore, efforts to mitigate the need for reoperation could be targeted towards optimizing the type of bone graft used, among other intraoperative variables.
Methods: Patients between January 2000 – December 2020 who underwent revision surgery for durotomy repair at a single institution were identified utilizing CPT codes for common sequelae. Patients were excluded if they were under the age of 18. Demographic information that were analyzed include patient age, gender, body mass index, and previous spine surgery. Intraoperative data included blood loss and operative time.
Results: Among the 106 patients with incidental durotomies, 7.5% had a re-leak and required re-operation for repair. Those with re-leaks had a higher incidence of steroid use (62.5% vs. 27.6%; p=0.05) and longer length of stay after surgery (10.5 days vs. 6.6 days; p=0.008). There was a statistically significant difference between the types of bone graft used for primary surgery (p=0.02), grafts used for durotomy repair (p=0.004), and borderline significance in days of bedrest (p=0.06) between those with re-leaks and those without. There was no statistical difference in Oswestry Disability Index (p=0.4) between the two groups.
Conclusion : As data collection on this patient population continues, it is becoming evident that patients who undergo reoperation do not have significantly worsened neurological function, but do experience significantly prolonged length of stay. Therefore, efforts to mitigate the need for reoperation could be targeted towards optimizing the type of bone graft used, among other intraoperative variables.
