Clinical Characterization of Larger Macroadenomas
Friday, April 21, 2023
- BH
Brian Hilton
Medical Student
Yale School of Medicine
ePoster Presenter(s)
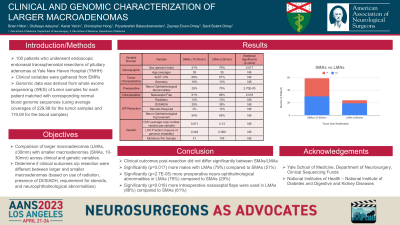
Introduction: We compared larger macroadenomas (LMAs, ≥30mm) with smaller macroadenomas (SMAs, 10-30mm) across clinical and genetic variables.
Methods: We examined clinical and genomic data that exists for 83 patients who underwent tumor resection of pituitary macroadenomas.
Results: Of this cohort, 71% (n=59) had LMAs and 29% (n=24) had SMAs. 79% (n=21) of LMAs were male compared to 51% (n=30) of SMAs (p=0.017). Both groups shared an average of 55 years old. 67% (n=16) of LMAs and 69% (n=41) of SMAs had a Ki-67 < 3%. 13% (n=3) of LMAs and 19% (n=11) of SMAs were secretory. 88% (n=21) of LMAs required nasoseptal flap compared to 61% (n=36) of SMAs, with statistical significance (p=0.018).
Focal radiation therapy was eventually administered to 13% (n=3) of LMAs and 14% (n=8) of SMAs, secondary to recurrence/residual. Temporary postoperative DI/SIADH occurred in 38% (n=9) for LMAs and 29% (n=17) for SMAs. New steroid replacement was required in 13% (n=2) of LMAs and 3% (n=1) of SMAs. These results did not show statistical significance.
79% (n=19) of LMAs had neuro-ophthalmological abnormalities compared to 29% (n=17) of SMAs (p= 2.7*10-5), preoperatively. Postoperatively, 95% (n=18) of LMAs and 94% (n=16) of SMAs experienced an improvement.
Somatic CNV, SNV/INDEL count, and genomic instability metrics did not show any statistically significant difference based on tumor size. For average CNV and LOH fractions, SMAs were respectively 0.071 and 0.048 compared to 0.13 and 0.069 for LMAs. On average, there were 41 mutations per sample for SMAs compared to 104 for LMAs. For mean blood and tumor coverages, SMAs were respectively 117.46 and 230.92 compared to 121.91 and 238.2 for LMAs.
Conclusion : The clinical outcomes post-resection did not differ significantly between SMAs and LMAs. Sex, preoperative neuro-ophthalmological abnormalities, and use of nasoseptal flap differed significantly.
Methods: We examined clinical and genomic data that exists for 83 patients who underwent tumor resection of pituitary macroadenomas.
Results: Of this cohort, 71% (n=59) had LMAs and 29% (n=24) had SMAs. 79% (n=21) of LMAs were male compared to 51% (n=30) of SMAs (p=0.017). Both groups shared an average of 55 years old. 67% (n=16) of LMAs and 69% (n=41) of SMAs had a Ki-67 < 3%. 13% (n=3) of LMAs and 19% (n=11) of SMAs were secretory. 88% (n=21) of LMAs required nasoseptal flap compared to 61% (n=36) of SMAs, with statistical significance (p=0.018).
Focal radiation therapy was eventually administered to 13% (n=3) of LMAs and 14% (n=8) of SMAs, secondary to recurrence/residual. Temporary postoperative DI/SIADH occurred in 38% (n=9) for LMAs and 29% (n=17) for SMAs. New steroid replacement was required in 13% (n=2) of LMAs and 3% (n=1) of SMAs. These results did not show statistical significance.
79% (n=19) of LMAs had neuro-ophthalmological abnormalities compared to 29% (n=17) of SMAs (p= 2.7*10-5), preoperatively. Postoperatively, 95% (n=18) of LMAs and 94% (n=16) of SMAs experienced an improvement.
Somatic CNV, SNV/INDEL count, and genomic instability metrics did not show any statistically significant difference based on tumor size. For average CNV and LOH fractions, SMAs were respectively 0.071 and 0.048 compared to 0.13 and 0.069 for LMAs. On average, there were 41 mutations per sample for SMAs compared to 104 for LMAs. For mean blood and tumor coverages, SMAs were respectively 117.46 and 230.92 compared to 121.91 and 238.2 for LMAs.
Conclusion : The clinical outcomes post-resection did not differ significantly between SMAs and LMAs. Sex, preoperative neuro-ophthalmological abnormalities, and use of nasoseptal flap differed significantly.
