Immunocompetent Neural Organoids Respond to Blood Stimulation: A Novel Model of Intracerebral Hemorrhage
Friday, April 21, 2023

Braxton R. Schuldt, BA
Medical Student
Icahn School of Medicine at Mount Sinai
New York, New York, United States
ePoster Presenter(s)
Introduction: The lack of treatments for intracerebral hemorrhage (ICH) suggests the need for novel preclinical models of this disease. To that end, this study aimed to explore the utility of an ICH neural organoid model.
Methods: Multicellular, microglia-containing human neural organoids were provided by Stem Pharm, Inc. On DIV 21, organoids were treated with human whole blood (n=3 organoids in each blood condition) for 24 hours. To serve as positive and negative controls, one organoid was treated with lipopolysaccharide (LPS) for 24 hours and three remained untreated. Human IL-6 concentrations were measured in the culture media prior to and after treatments using an enzyme-linked immunosorbent assay (ELISA) and the fold-change from baseline was normalized to the negative control condition. A one-way ANOVA with Dunnett’s test was performed to compare IL-6 secretion between the control and treatment conditions.
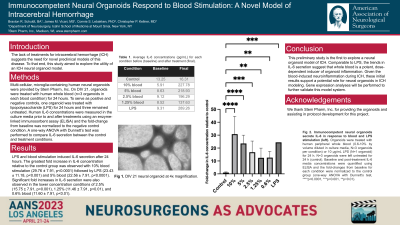
Results: LPS and blood stimulation induced IL-6 secretion after 24 hours. The greatest fold increase in IL-6 concentration relative to the control group was observed with 10% blood stimulation (29.76 ± 7.91, p< 0.0001) followed by LPS (23.43 ± 11.18, p< 0.001) and 5% blood (22.56 ± 7.91, p< 0.0001). Significant fold increases in IL-6 secretion were also observed in the lower concentration conditions of 2.5% (15.75 ± 7.91, p< 0.001), 1.25% (11.46 ± 7.91, p< 0.01), and 0.6% blood (11.60 ± 7.91, p< 0.01).
Conclusion : This preliminary study is the first to explore a neural organoid model of ICH. Comparable to LPS, the trends in IL-6 secretion suggest that whole blood is a potent, dose-dependent inducer of organoid inflammation. Given the blood-induced neuroinflammation during ICH, these initial results support a potential role for neural organoids in ICH modeling. Gene expression analyses will be performed to further validate this model system.
Methods: Multicellular, microglia-containing human neural organoids were provided by Stem Pharm, Inc. On DIV 21, organoids were treated with human whole blood (n=3 organoids in each blood condition) for 24 hours. To serve as positive and negative controls, one organoid was treated with lipopolysaccharide (LPS) for 24 hours and three remained untreated. Human IL-6 concentrations were measured in the culture media prior to and after treatments using an enzyme-linked immunosorbent assay (ELISA) and the fold-change from baseline was normalized to the negative control condition. A one-way ANOVA with Dunnett’s test was performed to compare IL-6 secretion between the control and treatment conditions.
Results: LPS and blood stimulation induced IL-6 secretion after 24 hours. The greatest fold increase in IL-6 concentration relative to the control group was observed with 10% blood stimulation (29.76 ± 7.91, p< 0.0001) followed by LPS (23.43 ± 11.18, p< 0.001) and 5% blood (22.56 ± 7.91, p< 0.0001). Significant fold increases in IL-6 secretion were also observed in the lower concentration conditions of 2.5% (15.75 ± 7.91, p< 0.001), 1.25% (11.46 ± 7.91, p< 0.01), and 0.6% blood (11.60 ± 7.91, p< 0.01).
Conclusion : This preliminary study is the first to explore a neural organoid model of ICH. Comparable to LPS, the trends in IL-6 secretion suggest that whole blood is a potent, dose-dependent inducer of organoid inflammation. Given the blood-induced neuroinflammation during ICH, these initial results support a potential role for neural organoids in ICH modeling. Gene expression analyses will be performed to further validate this model system.
