Association Between Surgeon Specialty and Outcomes after Spine Surgery: A Single Institution, Propensity-Matched Analysis of 3,023 Patients
Association Between Surgeon Specialty and Outcomes After Spine Surgery: A Single Institution, Propensity-matched Analysis of 3,023 Patients
Friday, April 21, 2023

Alexander Fabiano, BS
Medical Student
UT Southwestern
ePoster Presenter(s)
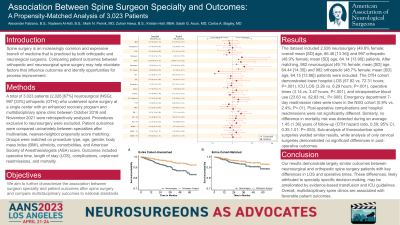
Introduction: Recent studies report specialty-specific differences in spine surgery outcomes. However, these studies utilized national databases which do not account for practice setting, patient characteristics, or availability of perioperative programs. We aim to assess the association of surgeon specialty with postoperative outcomes at an academic institution with a multidisciplinary spine team.
Methods: A total of 3,023 patients (2,026 [67%] neurosurgical (NSG); 997 [33%] orthopedic (OTH)) who underwent spine surgery at a single center with an enhanced recovery program and multidisciplinary spine clinic between October 2016 and November 2021 were retrospectively analyzed. Procedures exclusive to neurosurgery were excluded. Patient outcomes were compared univariately between specialties after multivariate, nearest-neighbor propensity score matching. Groups were matched on procedure type, age, gender, body mass index (BMI), ethnicity, comorbidities, and American Society of Anesthesiologists (ASA) score. Outcomes included operative time, length of stay (LOS), complications, unplanned readmissions, and mortality.
Results: After matching, 1,964 neurosurgical (mean [SD] age, 64.44 [14.35]) and orthopedic (mean [SD] age, 64.15 [13.86]) patients were included in the final analyses. BMI was the only significantly different matched characteristic (29.37 vs. 30.07 in OTH; P=.03). The OTH cohort demonstrated lower hospital LOS (57.82 vs. 72.31 hours; P < .001), ICU LOS (3.26 vs. 6.29 hours; P < .001), operative times (3.14 vs. 3.47 hours; P < .001), and intraoperative blood use (23.63 vs. 82.83 mL; P=.008). The association between OTH and 7-day ED readmissions strengthened (OR, 2.71; 95% CI, 1.3, 6.19; P=.01). Post-operative complications and hospital readmissions were not significantly different and OTH was not associated with a higher risk of mortality (hazard ratio 0.59; 95% CI, 0.35, 1.01; P=.053).
Conclusion : Our results demonstrate largely similar outcomes between neurosurgical and orthopedic spine surgery patients with key differences in LOS and operative times. These differences, likely attributed to specialty specific decision-making, may be ameliorated by evidence-based transfusion and ICU guidelines.
Methods: A total of 3,023 patients (2,026 [67%] neurosurgical (NSG); 997 [33%] orthopedic (OTH)) who underwent spine surgery at a single center with an enhanced recovery program and multidisciplinary spine clinic between October 2016 and November 2021 were retrospectively analyzed. Procedures exclusive to neurosurgery were excluded. Patient outcomes were compared univariately between specialties after multivariate, nearest-neighbor propensity score matching. Groups were matched on procedure type, age, gender, body mass index (BMI), ethnicity, comorbidities, and American Society of Anesthesiologists (ASA) score. Outcomes included operative time, length of stay (LOS), complications, unplanned readmissions, and mortality.
Results: After matching, 1,964 neurosurgical (mean [SD] age, 64.44 [14.35]) and orthopedic (mean [SD] age, 64.15 [13.86]) patients were included in the final analyses. BMI was the only significantly different matched characteristic (29.37 vs. 30.07 in OTH; P=.03). The OTH cohort demonstrated lower hospital LOS (57.82 vs. 72.31 hours; P < .001), ICU LOS (3.26 vs. 6.29 hours; P < .001), operative times (3.14 vs. 3.47 hours; P < .001), and intraoperative blood use (23.63 vs. 82.83 mL; P=.008). The association between OTH and 7-day ED readmissions strengthened (OR, 2.71; 95% CI, 1.3, 6.19; P=.01). Post-operative complications and hospital readmissions were not significantly different and OTH was not associated with a higher risk of mortality (hazard ratio 0.59; 95% CI, 0.35, 1.01; P=.053).
Conclusion : Our results demonstrate largely similar outcomes between neurosurgical and orthopedic spine surgery patients with key differences in LOS and operative times. These differences, likely attributed to specialty specific decision-making, may be ameliorated by evidence-based transfusion and ICU guidelines.
