AM-PAC Scores Predict Short and Long-Term Outcomes Following Glioblastoma Resection
AM-PAC Scores Predict Short and Long-term Outcomes Following Glioblastoma Resection
Friday, April 21, 2023

Saket Myneni (he/him/his)
Medical Student
Johns Hopkins University School of Medicine
ePoster Presenter(s)
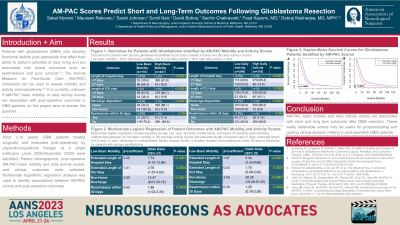
Introduction: Patients with glioblastoma (GBM) may develop functional deficits post-operatively that affect their ability to perform activities of daily living and are associated with worse outcomes such as readmissions and poor survival. The Activity Measure for Post-Acute Care (AM-PAC) assesses mobility and activity post-operatively, but it is unknown if these scores correlate with post-operative outcomes in GBM patients.
Methods: Adult (≥18 years) GBM patients treated surgically and evaluated post-operatively by physical/occupational therapy at a single instution (June 2008-December 2020) were identified. Patient demographics, post-operative AM-PAC scores, and clinical outcomes were collected. Multivariate regression analysis was used to identify associations between AM-PAC scores and post-operative outcomes.
Results: A total of 600 patients were included (mean age: 59.3 years, 59.2% male); 151 (25.3%) and 246 (43.8%) patients had low basic mobility ( < 42.9) and daily activity ( < 39.4) scores, respectively. A total of 103 (17.2%) and 177 (29.5%) patients experienced extended lengths of stay (LOS) in the ICU (≥2 days) and overall (≥7 days), respectively, and 154 (25.7%) patients had non-home discharge dispositions. The 30-day readmission rate was 13.7% (n=82).
In multivariate analysis, low AM-PAC basic mobility scores were associated with increased odds of overall extended LOS (p < 0.0001), extended ICU LOS (p=0.0004), non-home discharge (p < 0.0001), and 30-day readmission (p=0.0405). Low daily activity scores were independently associated with overall extended LOS ( < 0.0001) and non-home discharge (p < 0.0001). Patients with low basic mobility or low daily activity scores had shorter median overall survival times (9.5 and 10.6 months, respectively) than patients with high basic mobility (14.7 months, p< 0.0001) or high daily activity (16.3 months, p< 0.0001) scores in log-rank analysis.
Conclusion : AM-PAC mobility and activity scores are associated with short and long-term outcomes after GBM resection. These easily obtainable scores may be useful for prognosticating and guiding clinical decision making in post-operative GBM patients.
Methods: Adult (≥18 years) GBM patients treated surgically and evaluated post-operatively by physical/occupational therapy at a single instution (June 2008-December 2020) were identified. Patient demographics, post-operative AM-PAC scores, and clinical outcomes were collected. Multivariate regression analysis was used to identify associations between AM-PAC scores and post-operative outcomes.
Results: A total of 600 patients were included (mean age: 59.3 years, 59.2% male); 151 (25.3%) and 246 (43.8%) patients had low basic mobility ( < 42.9) and daily activity ( < 39.4) scores, respectively. A total of 103 (17.2%) and 177 (29.5%) patients experienced extended lengths of stay (LOS) in the ICU (≥2 days) and overall (≥7 days), respectively, and 154 (25.7%) patients had non-home discharge dispositions. The 30-day readmission rate was 13.7% (n=82).
In multivariate analysis, low AM-PAC basic mobility scores were associated with increased odds of overall extended LOS (p < 0.0001), extended ICU LOS (p=0.0004), non-home discharge (p < 0.0001), and 30-day readmission (p=0.0405). Low daily activity scores were independently associated with overall extended LOS ( < 0.0001) and non-home discharge (p < 0.0001). Patients with low basic mobility or low daily activity scores had shorter median overall survival times (9.5 and 10.6 months, respectively) than patients with high basic mobility (14.7 months, p< 0.0001) or high daily activity (16.3 months, p< 0.0001) scores in log-rank analysis.
Conclusion : AM-PAC mobility and activity scores are associated with short and long-term outcomes after GBM resection. These easily obtainable scores may be useful for prognosticating and guiding clinical decision making in post-operative GBM patients.
