Implementation of hypofractionated Gamma Knife radiosurgery to improve tumor control and toxicity in large brain metastasis
Implementation of Hypofractionated Gamma Knife Radiosurgery to Improve Tumor Control and Toxicity in Large Brain Metastasis
Friday, April 21, 2023

Akash Mishra
Medical Student
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell
ePoster Presenter(s)
Introduction: Brain metastases greater than 3cm in diameter are limited to 15Gy single-fraction SRS due to risk of radionecrosis, but this yields poor local control. Literature describing utilization of hypofractionated SRS for the treatment of large metastatic brain neoplasms is scarce. We report our experience using the Gamma Knife (GK) Icon to deliver hypofractionated treatment to large brain metastases. We present our clinical outcomes and identify clinical/treatment parameters that may have prognostic value.
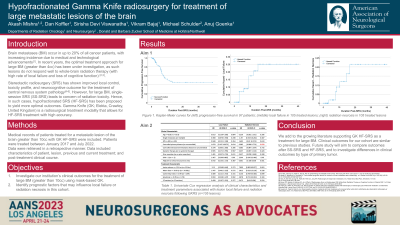
Methods: We retrospectively identified patients who received hypofractionated Gamma Knife radiosurgery (HF-GKRS) between 2017 and 2022 for the treatment of metastatic brain tumors greater than 10cc. Clinical, treatment, and radiological data was collected. Local failure (LF) and radionecrosis (RN) events were identified, and Kaplan-Meier curves of LF and RN were generated.
Results: Ninety-seven patients were treated for a total of 105 lesions greater than 10cc, and median follow-up was 10.1 months. The median gross tumor volume was 15.8cc (range 10.1-62.4), and no PTV margin was added. The most common tumor subtypes included lung (n=33 lesions) and breast (n=17). Six- and 12-month LF rates were 8.5 +/ 3.6% and 18.6 +/ 5.8%; comparable RN rates were 1.8 +/ 1.8% and 11.3 +/ 4.8%. Prior surgical resection was performed on 55 lesions (51.9%), but this did not correlate with LF (p = 0.969) or RN (p = 0.919).
Conclusion : We present our institutional experience treating large brain metastases greater than 10 cc using mask-based HF-GKRS typically to a dose of 27Gy in 3 fractions, representing one of the largest reported in the literature. Our data is unique in that we typically do not add a PTV margin when prescribing SRS. Our tumor control rates and toxicity outcomes compare quite favorably with the literature, supporting our practice.
Methods: We retrospectively identified patients who received hypofractionated Gamma Knife radiosurgery (HF-GKRS) between 2017 and 2022 for the treatment of metastatic brain tumors greater than 10cc. Clinical, treatment, and radiological data was collected. Local failure (LF) and radionecrosis (RN) events were identified, and Kaplan-Meier curves of LF and RN were generated.
Results: Ninety-seven patients were treated for a total of 105 lesions greater than 10cc, and median follow-up was 10.1 months. The median gross tumor volume was 15.8cc (range 10.1-62.4), and no PTV margin was added. The most common tumor subtypes included lung (n=33 lesions) and breast (n=17). Six- and 12-month LF rates were 8.5 +/ 3.6% and 18.6 +/ 5.8%; comparable RN rates were 1.8 +/ 1.8% and 11.3 +/ 4.8%. Prior surgical resection was performed on 55 lesions (51.9%), but this did not correlate with LF (p = 0.969) or RN (p = 0.919).
Conclusion : We present our institutional experience treating large brain metastases greater than 10 cc using mask-based HF-GKRS typically to a dose of 27Gy in 3 fractions, representing one of the largest reported in the literature. Our data is unique in that we typically do not add a PTV margin when prescribing SRS. Our tumor control rates and toxicity outcomes compare quite favorably with the literature, supporting our practice.
