Association of Patient Race/Ethnicity with Laser Interstitial Thermal Therapy Referral Patterns at a Single Center
Association of Patient Race/ethnicity with Laser Interstitial Thermal Therapy Referral Patterns at a Single Center
Friday, April 21, 2023
Has Audio

Aden P. Haskell-Mendoza, MS (he/him/his)
Medical Student
Duke University School of Medicine
Durham, North Carolina, United States
ePoster Presenter(s)
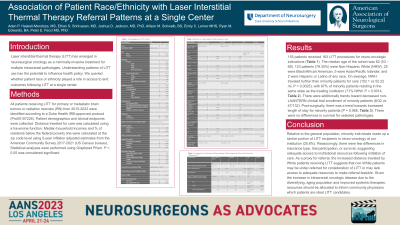
Introduction: Laser interstitial thermal therapy (LITT) has emerged in neurosurgical oncology as a minimally-invasive treatment for multiple intracranial pathologies. Understanding patterns of LITT use has the potential to influence health policy. We thus queried whether patient race or ethnicity played a role in access to LITT at a single center.
Methods: All patients receiving LITT for biopsy-confirmed brain tumors or radiation necrosis (RN) from 2015-2019 were identified according to a Duke Health IRB-approved protocol (Pro00107226). Patient demographics and clinical endpoints were collected. Distance traveled for care was calculated using a haversine function; statistical analyses were performed using Graphpad Prism.
Results: Sixty-eight patients received LITT. 34 (50%) identified as female. Thirty-four patients had RN, 17 had recurrent metastases, and 7 and 10 had newly-diagnosed or recurrent gliomas, respectively. 54 patients identified as White, while 12 identified as non-White (Black/African American, Asian, Native American, or Pacific Islander/Native Hawaiian) or Hispanic/Latino (NWHIs). Mean age for White patients was 58.9 vs 55.25 years for NWHIs, P=0.41. Similarly, mean KPS was 81.55 vs 82.50 for Whites vs NWHIs, P=0.79. There was no significant difference in comorbidities, insurance status, non-LITT clinical investigation participation, or post-LITT survival for Whites vs NWHIs. Surprisingly, the mean distance traveled by Whites was significantly greater than NWHIs, at 134.0 vs 33.49 miles, P=0.046.
Conclusion : Relative to the general population, NWHIs made up a smaller portion of LITT recipients at our institution (17.6%). Reassuringly, there were no differences in insurance, trial participation, or survival, suggesting adequate access to institutional resources following initiation of care. As a proxy for referral, the increased distance traveled by White patients receiving LITT suggests that non-White patients may be under-referred for consideration of LITT or may lack access to adequate resources to make referral feasible. Future resources could be allocated to inform local physicians which patients are ideal LITT candidates.
Methods: All patients receiving LITT for biopsy-confirmed brain tumors or radiation necrosis (RN) from 2015-2019 were identified according to a Duke Health IRB-approved protocol (Pro00107226). Patient demographics and clinical endpoints were collected. Distance traveled for care was calculated using a haversine function; statistical analyses were performed using Graphpad Prism.
Results: Sixty-eight patients received LITT. 34 (50%) identified as female. Thirty-four patients had RN, 17 had recurrent metastases, and 7 and 10 had newly-diagnosed or recurrent gliomas, respectively. 54 patients identified as White, while 12 identified as non-White (Black/African American, Asian, Native American, or Pacific Islander/Native Hawaiian) or Hispanic/Latino (NWHIs). Mean age for White patients was 58.9 vs 55.25 years for NWHIs, P=0.41. Similarly, mean KPS was 81.55 vs 82.50 for Whites vs NWHIs, P=0.79. There was no significant difference in comorbidities, insurance status, non-LITT clinical investigation participation, or post-LITT survival for Whites vs NWHIs. Surprisingly, the mean distance traveled by Whites was significantly greater than NWHIs, at 134.0 vs 33.49 miles, P=0.046.
Conclusion : Relative to the general population, NWHIs made up a smaller portion of LITT recipients at our institution (17.6%). Reassuringly, there were no differences in insurance, trial participation, or survival, suggesting adequate access to institutional resources following initiation of care. As a proxy for referral, the increased distance traveled by White patients receiving LITT suggests that non-White patients may be under-referred for consideration of LITT or may lack access to adequate resources to make referral feasible. Future resources could be allocated to inform local physicians which patients are ideal LITT candidates.
