Defining Appropriate Invasiveness Thresholds Within Different Frailty and Deformity Severity States for Surgical Intervention Among ASD Patients
Friday, April 21, 2023

Peter G. Passias, MD
Spine Surgeon
NYU School of Medicine
New Canaan, CT, US
ePoster Presenter(s)
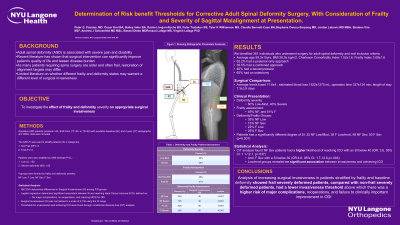
Introduction: As many patients requiring spine surgery are elder and often frail, restoration of alignment targets may differ. There is paucity in literature on whether different frailty and deformity states may warrant a different level of surgical invasiveness.
Methods: Operative ASD patients were included and categorized by Frailty into: Not Frail (NF), and Frail (F) and stratified by PILL as Severe deformity (Sev): >20, and Low (Low): < 20. 4 groups were formed: NF Low, F Low, NF Sev, F Sev. Thresholds for invasiveness level and cost utility were found through conditional inference tree (CIT) machine learning. Costs were calculated using the PearlDiver database, with QALY being calculated from SF6D.
Results: 381 patients were groups as: 44% NF Low, 19% NF Sev, 13% F Low, 20% F Sev. Higher costs for frail groups is likely due to an increased rate of revisions (p= < .001). The QALY gained by 2Y was: NF Low-.14, F Low-.22, NF Sev-.15, F Sev-.28 (p < .01). Despite higher surgical costs for F groups, the greater amount of QALY gained resulted in a justifiable cost utility by 2Y compared with NF groups (NF Low- $538,812 F Low- $490,907, NF Sev- $647,801, F Sev- $384,596). CIT found cutoffs between invasiveness and cost utility:37 for NF LM, 23 for F LM.
Conclusion : Cost analysis shows cost utility is at least for frail patients across both low and high degrees of deformity. Higher surgical costs, including higher rates of complications, by 2 years for frail patients are offset by the quality-adjusted life years gained by 2 years. When looking at surgical invasiveness, a lower degree of surgical invasiveness for frail patients maintains cost utility comparable to not frail patient. It is important to note this is a parabolic relationship and severe frailty has substantially greater surgical costs and lower cost-utility.
Methods: Operative ASD patients were included and categorized by Frailty into: Not Frail (NF), and Frail (F) and stratified by PILL as Severe deformity (Sev): >20, and Low (Low): < 20. 4 groups were formed: NF Low, F Low, NF Sev, F Sev. Thresholds for invasiveness level and cost utility were found through conditional inference tree (CIT) machine learning. Costs were calculated using the PearlDiver database, with QALY being calculated from SF6D.
Results: 381 patients were groups as: 44% NF Low, 19% NF Sev, 13% F Low, 20% F Sev. Higher costs for frail groups is likely due to an increased rate of revisions (p= < .001). The QALY gained by 2Y was: NF Low-.14, F Low-.22, NF Sev-.15, F Sev-.28 (p < .01). Despite higher surgical costs for F groups, the greater amount of QALY gained resulted in a justifiable cost utility by 2Y compared with NF groups (NF Low- $538,812 F Low- $490,907, NF Sev- $647,801, F Sev- $384,596). CIT found cutoffs between invasiveness and cost utility:37 for NF LM, 23 for F LM.
Conclusion : Cost analysis shows cost utility is at least for frail patients across both low and high degrees of deformity. Higher surgical costs, including higher rates of complications, by 2 years for frail patients are offset by the quality-adjusted life years gained by 2 years. When looking at surgical invasiveness, a lower degree of surgical invasiveness for frail patients maintains cost utility comparable to not frail patient. It is important to note this is a parabolic relationship and severe frailty has substantially greater surgical costs and lower cost-utility.
