Development of a Modified Surgical Invasiveness Index for Minimally-Invasive Adult Spinal Deformity Surgery
Development of a Modified Surgical Invasiveness Index for Minimally-invasive Adult Spinal Deformity Surgery
Friday, April 21, 2023

Peter G. Passias, MD
Spine Surgeon
NYU School of Medicine
New Canaan, CT, US
ePoster Presenter(s)
Introduction: Minimally Invasive Spine Surgery (MISS) techniques in ASD surgery may provide benefit to patients unable to tolerate traditional open technique. Despite increasing overlap between the abilities of open and MIS technique, no invasiveness index exists for MISS.
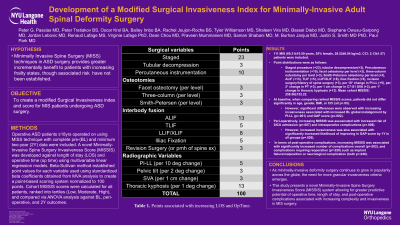
Methods: Operative ASD patients ≥18yrs operated on using MISS technique with complete pre-(BL) and two-year (2Y) data were included. A novel Minimally-Invasive Spine Surgery Invasiveness Score (MISSIS) was developed against length of stay (LOS) and operative time (op time) using multivariable regression models. Beta-Sullivan method established point values using standardized beta coefficients obtained from MVA analysis to create a point-based scoring system normalized to 100 points. Cohort MISSIS scores were calculated for all patients, ranked into tertiles (Low, Moderate, High), and compared via ANOVA analysis against BL, peri-operative, and 2Y outcomes.
Results: 111 MIS (69.31±10.59 years, 55% female, 28.52±6.04 kg/m2, CCI: 2.13±1.57) patients were included. Point distributions: Staged procedure (+23), tubular decompression(+3), Percutaneous instrumentation (+10), facet osteotomy per level (+3), three-column osteotomy per level (+3), Smith-Peterson osteotomy per level (+3), ALIF (+13), TLIF (+5), LLIF/XLIF (+8), iliac fixation (+5), revision surgery/history of spine surgery (+3), per 10° change in PI-LL (+5), per 2° change in PT (+3), per 1 cm change in C7-S1 SVA (+3), per 1° change in thoracic kyphosis (+13). Mean cohort MISSIS: 258.56±152.22. Peri-operatively, increasing MISSIS was associated with increased risk of intraoperative complications (p=.008). Post-operatively, increasing MISSIS was associated with increased complications overall (p=.002) and reoperation (p=.020), and implant failure/malposition or neurological complication (both p < .046).
Conclusion : As minimally-invasive deformity surgery continues to grow in popularity across the globe, the need for more granular invasiveness criteria emerges. This study presents a novel Minimally-Invasive Spine Surgery Invasiveness Score (MISSIS) system allowing for greater predictive potential of operative time, length of stay, and post-operative complications associated with increasing complexity and invasiveness in MIS surgery.
Methods: Operative ASD patients ≥18yrs operated on using MISS technique with complete pre-(BL) and two-year (2Y) data were included. A novel Minimally-Invasive Spine Surgery Invasiveness Score (MISSIS) was developed against length of stay (LOS) and operative time (op time) using multivariable regression models. Beta-Sullivan method established point values using standardized beta coefficients obtained from MVA analysis to create a point-based scoring system normalized to 100 points. Cohort MISSIS scores were calculated for all patients, ranked into tertiles (Low, Moderate, High), and compared via ANOVA analysis against BL, peri-operative, and 2Y outcomes.
Results: 111 MIS (69.31±10.59 years, 55% female, 28.52±6.04 kg/m2, CCI: 2.13±1.57) patients were included. Point distributions: Staged procedure (+23), tubular decompression(+3), Percutaneous instrumentation (+10), facet osteotomy per level (+3), three-column osteotomy per level (+3), Smith-Peterson osteotomy per level (+3), ALIF (+13), TLIF (+5), LLIF/XLIF (+8), iliac fixation (+5), revision surgery/history of spine surgery (+3), per 10° change in PI-LL (+5), per 2° change in PT (+3), per 1 cm change in C7-S1 SVA (+3), per 1° change in thoracic kyphosis (+13). Mean cohort MISSIS: 258.56±152.22. Peri-operatively, increasing MISSIS was associated with increased risk of intraoperative complications (p=.008). Post-operatively, increasing MISSIS was associated with increased complications overall (p=.002) and reoperation (p=.020), and implant failure/malposition or neurological complication (both p < .046).
Conclusion : As minimally-invasive deformity surgery continues to grow in popularity across the globe, the need for more granular invasiveness criteria emerges. This study presents a novel Minimally-Invasive Spine Surgery Invasiveness Score (MISSIS) system allowing for greater predictive potential of operative time, length of stay, and post-operative complications associated with increasing complexity and invasiveness in MIS surgery.
