Defining a High Risk Adult Spinal Deformity Patient
Friday, April 21, 2023

Peter G. Passias, MD
Spine Surgeon
NYU School of Medicine
New Canaan, CT, US
ePoster Presenter(s)
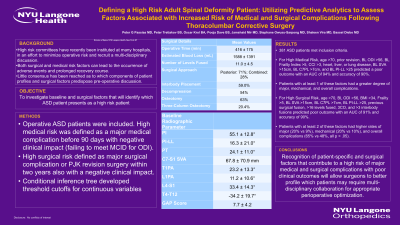
Introduction: High risk committees have recently been instituted at many hospitals, in an effort to minimize operative risk and recruit a multi-disciplinary discussion. Both surgical and medical risk factors can lead to the occurrence of adverse events and prolonged recovery course. Little consensus has been reached as to which components of patient profiles and surgical factors predispose pre-operative discussion.
Methods: Operative ASD patients were included. High medical risk was defined as a major medical complication before 90 days with negative clinical impact (failing to meet MCID for ODI). High surgical risk defined as major surgical complication or PJK revision surgery within two years also with a negative clinical impact. Conditional inference tree developed threshold cutoffs for continuous variables.
Results: 381 ASD patients met inclusion criteria. For High Medical Risk, age >70, prior revision, BL ODI >56, BL Frailty Index >5, CCI >3, heart, liver, or lung disease, BL SVA >15cm, BL C7PL >7cm, and BL PI-LL >25 predicted a poor outcome with an AUC of 94% and accuracy of 90%. Patients with at least 1 of these factors had a greater degree of major, mechanical, and overall complications. For High Surgical Risk, age >70, BL ODI >56, BMI >34, Frailty >5, BL SVA >15cm, BL C7PL >7cm, BL PI-LL >25, previous surgical fusion, >16 levels fused, 3CO, and >3 interbody fusions predicted poor outcome with an AUC of 91% and accuracy of 90%. Patients with at least 2 of these factors had higher rates of major (20% vs 9%), mechanical (20% vs 10%), and overall complications (65% vs 48%, all p < .05).
Conclusion : Recognition of patient-specific and surgical factors that contribute to a high risk of major medical and surgical complications with poor clinical outcomes will allow surgeons to better profile which patients may require multi-disciplinary collaboration for appropriate perioperative optimization.
Methods: Operative ASD patients were included. High medical risk was defined as a major medical complication before 90 days with negative clinical impact (failing to meet MCID for ODI). High surgical risk defined as major surgical complication or PJK revision surgery within two years also with a negative clinical impact. Conditional inference tree developed threshold cutoffs for continuous variables.
Results: 381 ASD patients met inclusion criteria. For High Medical Risk, age >70, prior revision, BL ODI >56, BL Frailty Index >5, CCI >3, heart, liver, or lung disease, BL SVA >15cm, BL C7PL >7cm, and BL PI-LL >25 predicted a poor outcome with an AUC of 94% and accuracy of 90%. Patients with at least 1 of these factors had a greater degree of major, mechanical, and overall complications. For High Surgical Risk, age >70, BL ODI >56, BMI >34, Frailty >5, BL SVA >15cm, BL C7PL >7cm, BL PI-LL >25, previous surgical fusion, >16 levels fused, 3CO, and >3 interbody fusions predicted poor outcome with an AUC of 91% and accuracy of 90%. Patients with at least 2 of these factors had higher rates of major (20% vs 9%), mechanical (20% vs 10%), and overall complications (65% vs 48%, all p < .05).
Conclusion : Recognition of patient-specific and surgical factors that contribute to a high risk of major medical and surgical complications with poor clinical outcomes will allow surgeons to better profile which patients may require multi-disciplinary collaboration for appropriate perioperative optimization.
