Extended Survivals in the Care of Breast Cancer Brain Metastases Patients after Stereotactic Radiosurgery
Extended Survivals in the Care of Breast Cancer Brain Metastases Patients After Stereotactic Radiosurgery
Friday, April 21, 2023
Has Audio

Elad Mashiach, MS (he/him/his)
Medical Student
NYU Langone Health
ePoster Presenter(s)
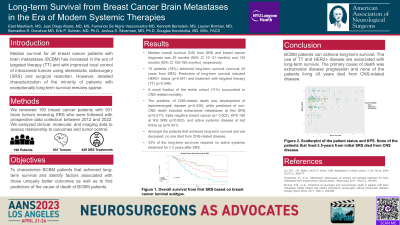
Introduction: With the advent of targeted systemic therapy, breast cancer patients with brain metastases (BCBM) are reported to have increased overall survival. The aim of this project is to explore predictors of overall survival (OS), local failure, and distant failure in current care paradigms. In prior decades, overall median survivals were in the order of one year.
Methods: We used our prospective patient registry to evaluate data from 2012-2022. We included BCBM patients who received gamma knife stereotactic radiosurgery (SRS) with a minimum of three-months imaging follow-up. In total, 50 recent patients with 257 tumors were included. Local control (LC) was determined using the RANO criteria. Survival was estimated using the Kaplan-Meier method and hazard ratios were calculated using Cox proportional hazards model.
Results: The median age was 56 years, and the median number of tumors per patient was 2. Local failure was reported in 25 out of 257 tumors (9.7%). LC rates were 93%, 89%, 81% at 12, 24, and 48 months, respectively. LC rates based on luminal type at 12 months are 62%, 78%, 89%, 100% for basal, HER2, luminal A, and luminal B, respectively. New remote brain metastases were found in 60% and 78% at 12 and 24 months, respectively. Number of BM at diagnosis was associated with higher frequency of distant failure (HR 1.056 CI= 1.005-1.108, P=0.029). The median OS was 35 months. HER2+ subtype was associated with increased OS compared to HER2- subtype at 36 months, 63% and 23%, respectively (P=0.042). Conversely, active systemic disease status at last follow up was associated with decreased OS (HR 2.542 CI=1.047-6.173 P=0.039). Symptomatic adverse radiation events (AREs) were reported in 4 patients (8%).
Conclusion : SRS for the treatment of BCBM is associated with high LC rates with significant expectations for extended median survivals now approaching 3 years, particularly for HER2+ patients.
Methods: We used our prospective patient registry to evaluate data from 2012-2022. We included BCBM patients who received gamma knife stereotactic radiosurgery (SRS) with a minimum of three-months imaging follow-up. In total, 50 recent patients with 257 tumors were included. Local control (LC) was determined using the RANO criteria. Survival was estimated using the Kaplan-Meier method and hazard ratios were calculated using Cox proportional hazards model.
Results: The median age was 56 years, and the median number of tumors per patient was 2. Local failure was reported in 25 out of 257 tumors (9.7%). LC rates were 93%, 89%, 81% at 12, 24, and 48 months, respectively. LC rates based on luminal type at 12 months are 62%, 78%, 89%, 100% for basal, HER2, luminal A, and luminal B, respectively. New remote brain metastases were found in 60% and 78% at 12 and 24 months, respectively. Number of BM at diagnosis was associated with higher frequency of distant failure (HR 1.056 CI= 1.005-1.108, P=0.029). The median OS was 35 months. HER2+ subtype was associated with increased OS compared to HER2- subtype at 36 months, 63% and 23%, respectively (P=0.042). Conversely, active systemic disease status at last follow up was associated with decreased OS (HR 2.542 CI=1.047-6.173 P=0.039). Symptomatic adverse radiation events (AREs) were reported in 4 patients (8%).
Conclusion : SRS for the treatment of BCBM is associated with high LC rates with significant expectations for extended median survivals now approaching 3 years, particularly for HER2+ patients.
