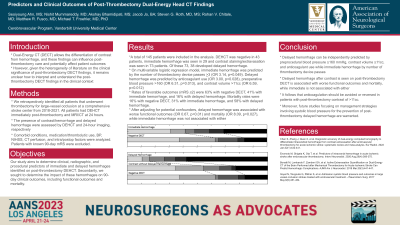
Predictors and Clinical Outcomes of Post-Thrombectomy Dual Energy Head CT Findings
Predictors and Clinical Outcomes of Post-thrombectomy Dual Energy Head CT Findings
Friday, April 21, 2023
Seoiyoung Ahn, MS (he/him/his)
Medical Student
Vanderbilt University School of Medicine
ePoster Presenter(s)
Introduction: Dual-energy head CT (DEHCT) allows the differentiation of contrast from hemorrhage, and these findings can influence post-thrombectomy care and potentially affect patient outcomes. Our study aims to determine clinical and radiographic predictors of immediate and delayed hemorrhages following thrombectomy and impact on 90-day outcomes.
Methods: We retrospectively identified all ischemic stroke patients that underwent thrombectomy at a comprehensive stroke center from 2018-2021. Per protocol, all patients had DEHCT post-thrombectomy and MRI or CT 24 hours afterward. The presence of contrast and/or hemorrhage was assessed by iodine maps and virtual non-contrast images of DEHCT. Delayed hemorrhage was determined by 24-hour imaging. Comorbid conditions, medication/thrombolytic use, blood pressure (BP), NIHSS, CT perfusion, and intraoperative factors were incorporated into univariate/multivariate logistic regression models.
Results: A total of 145 patients were included in the analysis. DEHCT was negative in 43, hemorrhage was seen in 29, and contrast was seen in 73 patients. Of the 73 with contrast on DEHCT, 38 underwent subsequent hemorrhagic transformation. Delayed hemorrhage was seen in one patient with negative DEHCT. On multivariate analyses, number of passes (OR3.14, p=0.049) predicted immediate hemorrhage, while anticoagulants (OR3.00, p=0.028), preoperative BP (OR6.31, p=0.013), and contrast volume (OR6.59, p=0.012) predicted delayed hemorrhage.
Rates of favorable functional outcomes (modified Rankin score ≤2) were 63% with negative DEHCT, 41% with immediate hemorrhage, and 16% with delayed hemorrhage. Mortality rates were 16% with negative DEHCT, 31% with immediate hemorrhage, and 58% with delayed hemorrhage. After adjusting for potential confounders, delayed hemorrhage was associated with worse functional outcomes (OR0.68, p< 0.001) and higher mortality (OR8.09, p=0.027) while immediate hemorrhage was not.
Conclusion : Delayed hemorrhage after contrast is seen on post-thrombectomy DEHCT is associated with worse functional outcomes and increased mortality, and can be predicted by anticoagulant use, elevated BP, and contrast volume. This information may guide the postoperative care of thrombectomy patients.
Methods: We retrospectively identified all ischemic stroke patients that underwent thrombectomy at a comprehensive stroke center from 2018-2021. Per protocol, all patients had DEHCT post-thrombectomy and MRI or CT 24 hours afterward. The presence of contrast and/or hemorrhage was assessed by iodine maps and virtual non-contrast images of DEHCT. Delayed hemorrhage was determined by 24-hour imaging. Comorbid conditions, medication/thrombolytic use, blood pressure (BP), NIHSS, CT perfusion, and intraoperative factors were incorporated into univariate/multivariate logistic regression models.
Results: A total of 145 patients were included in the analysis. DEHCT was negative in 43, hemorrhage was seen in 29, and contrast was seen in 73 patients. Of the 73 with contrast on DEHCT, 38 underwent subsequent hemorrhagic transformation. Delayed hemorrhage was seen in one patient with negative DEHCT. On multivariate analyses, number of passes (OR3.14, p=0.049) predicted immediate hemorrhage, while anticoagulants (OR3.00, p=0.028), preoperative BP (OR6.31, p=0.013), and contrast volume (OR6.59, p=0.012) predicted delayed hemorrhage.
Rates of favorable functional outcomes (modified Rankin score ≤2) were 63% with negative DEHCT, 41% with immediate hemorrhage, and 16% with delayed hemorrhage. Mortality rates were 16% with negative DEHCT, 31% with immediate hemorrhage, and 58% with delayed hemorrhage. After adjusting for potential confounders, delayed hemorrhage was associated with worse functional outcomes (OR0.68, p< 0.001) and higher mortality (OR8.09, p=0.027) while immediate hemorrhage was not.
Conclusion : Delayed hemorrhage after contrast is seen on post-thrombectomy DEHCT is associated with worse functional outcomes and increased mortality, and can be predicted by anticoagulant use, elevated BP, and contrast volume. This information may guide the postoperative care of thrombectomy patients.
