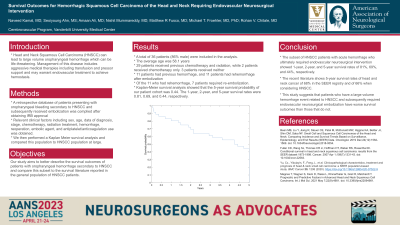
Survival Outcomes for Hemorrhagic Squamous Cell Carcinoma of the Head and Neck Requiring Endovascular Neurosurgical Intervention
Friday, April 21, 2023
Seoiyoung Ahn, MS (he/him/his)
Medical Student
Vanderbilt University School of Medicine
ePoster Presenter(s)
Introduction: Head and Neck Squamous Cell Carcinoma (HNSCC) can lead to large volume oropharyngeal hemorrhage which can be life-threatening. Management of this disease includes aggressive medical therapies including transfusion and pressor support and may warrant endovascular treatment to achieve hemostasis. Our study aims to better describe the survival outcomes of patients with oropharyngeal hemorrhage secondary to HNSCC and compare this subset to the survival literature reported in the general population of HNSCC patients.
Methods: A retrospective database of patients presenting with oropharyngeal bleeding secondary to HNSCC and subsequently received embolization was compiled after obtaining IRB approval. Relevant clinical factors including sex, age, date of diagnosis, stage, chemotherapy, radiation, rehemorrhage, reoperation, embolic agent, and antiplatelet/anticoagulation use was obtained. We then performed a Kaplan Meier survival analysis and compared this population to HNSCC population at large.
Results: A total of 36 patients (86% male) were included in the analysis. The average age was 58.1 years. 29 patients received previous chemotherapy and radiation, while 2 patients received chemotherapy only. 3 patients received neither. 11 patients had previous hemorrhage, and 11 patients had rehemorrhage after embolization. Of the 11 who had rehemorrhage, 7 patients required re-embolization. Kaplan Meier survival analysis showed that the 5-year survival probability of our patient cohort was 0.44. The 1- and 2-year survival rates were 0.81 and 0.69, respectively.
Conclusion : The subset of SCC patients with acute hemorrhage who ultimately required endovascular neurosurgical intervention showed 1-year, 2-year, and 5-year survival rates of 81%, 69%, and 44%, respectively. The recent literature shows 5-year survival rates of head and neck cancer of 68% in the SEER registry and of 66% when considering HNSCC. This suggests that patients who have a large-volume hemorrhage event related to HNSCC have worse survival outcomes than those that do not.
Methods: A retrospective database of patients presenting with oropharyngeal bleeding secondary to HNSCC and subsequently received embolization was compiled after obtaining IRB approval. Relevant clinical factors including sex, age, date of diagnosis, stage, chemotherapy, radiation, rehemorrhage, reoperation, embolic agent, and antiplatelet/anticoagulation use was obtained. We then performed a Kaplan Meier survival analysis and compared this population to HNSCC population at large.
Results: A total of 36 patients (86% male) were included in the analysis. The average age was 58.1 years. 29 patients received previous chemotherapy and radiation, while 2 patients received chemotherapy only. 3 patients received neither. 11 patients had previous hemorrhage, and 11 patients had rehemorrhage after embolization. Of the 11 who had rehemorrhage, 7 patients required re-embolization. Kaplan Meier survival analysis showed that the 5-year survival probability of our patient cohort was 0.44. The 1- and 2-year survival rates were 0.81 and 0.69, respectively.
Conclusion : The subset of SCC patients with acute hemorrhage who ultimately required endovascular neurosurgical intervention showed 1-year, 2-year, and 5-year survival rates of 81%, 69%, and 44%, respectively. The recent literature shows 5-year survival rates of head and neck cancer of 68% in the SEER registry and of 66% when considering HNSCC. This suggests that patients who have a large-volume hemorrhage event related to HNSCC have worse survival outcomes than those that do not.
