Comparison of Computed Tomography Angiogram and Digital Subtraction Angiogram in the Detection of Hemorrhage Source in Large Volume Head and Neck Bleeding
Friday, April 21, 2023
Seoiyoung Ahn, MS (he/him/his)
Medical Student
Vanderbilt University School of Medicine
ePoster Presenter(s)
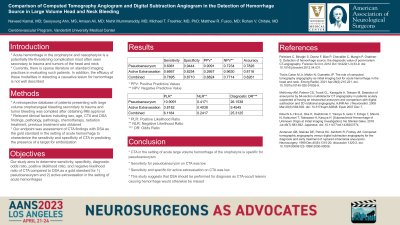
Introduction: Acute hemorrhage in the oropharynx and nasopharynx is a potentially life-threatening complication most often seen secondary to trauma and tumors of the head and neck. Currently there is sparse literature on standard imaging practices in evaluating such patients. In addition, the efficacy of these modalities in detecting a causative lesion for hemorrhage is not well described.
Methods: A retrospective database of patients presenting with large volume oropharyngeal bleeding secondary to trauma and tumor bleeding was compiled after obtaining IRB approval. Relevant clinical factors including sex, age, Computed Tomography Angiogram (CTA) findings, Digital Subtraction Angiography (DSA) findings, pathology, chemotherapy, radiation, and previous hemorrhage were obtained. Our primary endpoint was assessment of CTA findings with DSA as the gold standard in the setting of acute hemorrhage to characterize the sensitivity and specificity of CTA in predicting the presence of a target for embolization.
Results: A total of 69 patients (58% male) were included in this analysis. Of these, 56 (81%) had a tumor of the head and neck, predominantly squamous cell carcinoma. 12 (17.1%) patients had hemorrhage secondary to trauma. Sensitivity and specificity of CTA for pseudoaneurysm were 0.6061 and 0.9441 respectively. The diagnostic odds ratio (DOR) was 26.1538 with positive likelihood ratio (PLR) of 10.9091 and negative likelihood ratio (NLR) of 0.4171. For active extravasation, sensitivity and specificity of CTA were 0.6667 and 0.8254 respectively. The DOR of CTA for active extravasation was 9.4545 with PLR of 3.8182 and NLR of 0.4038.
Conclusion : CTA in the setting of acute large volume hemorrhage of the oropharynx is specific for pseudoaneurysm. Sensitivity for pseudoaneurysm on CTA was low and sensitivity and specificity for active extravasation on CTA were low. This suggests that DSA should be performed for diagnosis as CTA-occult lesions causing hemorrhage would otherwise be missed.
Methods: A retrospective database of patients presenting with large volume oropharyngeal bleeding secondary to trauma and tumor bleeding was compiled after obtaining IRB approval. Relevant clinical factors including sex, age, Computed Tomography Angiogram (CTA) findings, Digital Subtraction Angiography (DSA) findings, pathology, chemotherapy, radiation, and previous hemorrhage were obtained. Our primary endpoint was assessment of CTA findings with DSA as the gold standard in the setting of acute hemorrhage to characterize the sensitivity and specificity of CTA in predicting the presence of a target for embolization.
Results: A total of 69 patients (58% male) were included in this analysis. Of these, 56 (81%) had a tumor of the head and neck, predominantly squamous cell carcinoma. 12 (17.1%) patients had hemorrhage secondary to trauma. Sensitivity and specificity of CTA for pseudoaneurysm were 0.6061 and 0.9441 respectively. The diagnostic odds ratio (DOR) was 26.1538 with positive likelihood ratio (PLR) of 10.9091 and negative likelihood ratio (NLR) of 0.4171. For active extravasation, sensitivity and specificity of CTA were 0.6667 and 0.8254 respectively. The DOR of CTA for active extravasation was 9.4545 with PLR of 3.8182 and NLR of 0.4038.
Conclusion : CTA in the setting of acute large volume hemorrhage of the oropharynx is specific for pseudoaneurysm. Sensitivity for pseudoaneurysm on CTA was low and sensitivity and specificity for active extravasation on CTA were low. This suggests that DSA should be performed for diagnosis as CTA-occult lesions causing hemorrhage would otherwise be missed.
