Triggering T cell exhaustion in neuropsychiatric lupus prolongs survival and reduces T cell accumulation in the brain
Triggering T Cell Exhaustion in Neuropsychiatric Lupus Prolongs Survival and Reduces T Cell Accumulation in the Brain
Friday, April 21, 2023

Nancy Gonzalez (she/they)
MD/PhD Student
Texas A&M School of Medicine
Houston, Texas, United States
ePoster Presenter(s)
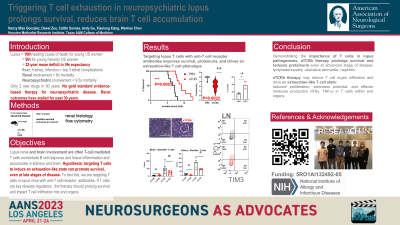
Introduction: Systemic Lupus Erythematosus (SLE) is a leading cause of death in young US women. Neuropsychiatric lupus (NPSLE), which can entail cerebral vasculitis, stroke, and even subarachnoid hemorrhage, is poorly understood. While NPSLE confers a 9.5-fold increase in mortality rate over the general population, it lacks gold standard, evidence-based treatment and is often excluded from SLE clinical trials. Only two drugs have been approved for SLE in the past 60 years, neither with known efficacy in NPSLE. On NPSLE autopsy, T and B cells infiltrate the choroid plexus. Moore et al. showed intracerebroventricular delivery of choroid plexus T cells worsened murine NPSLE (MRL.lpr). We hypothesize that anti-TCR beta antibody can trigger an exhaustion-like state in autoreactive T cells and thus reduce brain T cell infiltration and improve outcomes in lupus-prone MRL.lpr mice, even when initiated at advanced disease.
Methods: In the fourth month of life at advanced disease, we intraperitoneally injected mice with low-dose antiTCR beta antibodies once weekly for 5 weeks and then monitored survival. Next, in a pilot cohort, after three doses of anti-TCR antibody, treated and non-treated mice were sacked and PBS-perfused; brain-infiltrating T cells were analyzed by flow cytometry.
Results: Treated mice survived longer than controls (p=0.0007, Mantel-Cox, n=17). Pilot data from timed euthanasia post 3 anti-TCR doses showed reduced T cell accumulation in brains and kidney. T cells in the brains of treated mice showed an exhaustion-like phenotype, with reduced proliferation and effector molecule production.
Conclusion : These data highlight the power of modulating the autoreactive T cell response in lupus, to prolong life and reduce end-organ T cell accumulation. T cells warrant further exploration as a therapeutic target in NPSLE.
Methods: In the fourth month of life at advanced disease, we intraperitoneally injected mice with low-dose antiTCR beta antibodies once weekly for 5 weeks and then monitored survival. Next, in a pilot cohort, after three doses of anti-TCR antibody, treated and non-treated mice were sacked and PBS-perfused; brain-infiltrating T cells were analyzed by flow cytometry.
Results: Treated mice survived longer than controls (p=0.0007, Mantel-Cox, n=17). Pilot data from timed euthanasia post 3 anti-TCR doses showed reduced T cell accumulation in brains and kidney. T cells in the brains of treated mice showed an exhaustion-like phenotype, with reduced proliferation and effector molecule production.
Conclusion : These data highlight the power of modulating the autoreactive T cell response in lupus, to prolong life and reduce end-organ T cell accumulation. T cells warrant further exploration as a therapeutic target in NPSLE.
