Predictors of Mortality in Spondylodiscitis
Friday, April 21, 2023

John Paul G. Kolcun, MD
Resident Physician
Rush University Medical Center
ePoster Presenter(s)
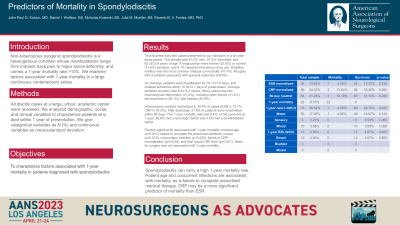
Introduction: Non-tuberculous pyogenic spondylodiscitis is a heterogenous condition whose manifestations range from indolent back pain to major spinal deformity, and carries a 1-year mortality rate >10%. We examine factors associated with 1-year mortality in the largest continuous series of discitis cases to-date.
Methods: All discitis cases at a large, urban, academic center were reviewed. We analyzed demographic, social, and clinical variables to characterize patients who died within 1 year of presentation. We give categorical variables as N (%) and continuous variables as mean±standard deviation.
Results: Two-hundred sixty-two cases presented to our institution in a six-year study period. The sample was 61.2% men, 51.0% minorities, and 62.2±13.9 years of age. A large portion were former (33.8%) or current (15.6%) smokers, and 9.1% reported intravenous drug use. Diabetes mellitus was the most common medical co-morbidity (41.4%). Roughly half of patients presented with epidural extension (50.6%).
On average, patients were hospitalized for 16.1±13.8 days, and initiated antibiotics within 10.9±12.1 days of presentation. Average antibiotic duration was 8.4±14.4 weeks. Many cases required neurosurgical intervention (47.2%), including open biopsy (41.4%), decompression (28.1%), and fixation (26.9%).
Inflammatory markers normalized in 39.8% of cases (ESR in 13.7%, CRP in 34.2%). After discharge, 31.9% of patients were re-admitted within 90 days. The 1-year mortality rate was 8.4%; of the survivors at 1-year, 26.6% had a neurologic deficit and 4.6% had a bowel/bladder deficit.
Factors significantly associated with 1-year mortality included age (p=0.010), failure to complete the prescribed antibiotic course (p=0.015), concomitant infection (p=0.005), failure of CRP normalization (p=0.038), and final actual CRP level (p=0.001). Need for surgery was not associated with 1-year mortality.
Conclusion : Spondylodiscitis can carry a high 1-year mortality rate. Patient age and concurrent infections are associated with mortality, as is failure to complete prescribed medical therapy. CRP may be a more significant predictor of mortality than ESR.
Methods: All discitis cases at a large, urban, academic center were reviewed. We analyzed demographic, social, and clinical variables to characterize patients who died within 1 year of presentation. We give categorical variables as N (%) and continuous variables as mean±standard deviation.
Results: Two-hundred sixty-two cases presented to our institution in a six-year study period. The sample was 61.2% men, 51.0% minorities, and 62.2±13.9 years of age. A large portion were former (33.8%) or current (15.6%) smokers, and 9.1% reported intravenous drug use. Diabetes mellitus was the most common medical co-morbidity (41.4%). Roughly half of patients presented with epidural extension (50.6%).
On average, patients were hospitalized for 16.1±13.8 days, and initiated antibiotics within 10.9±12.1 days of presentation. Average antibiotic duration was 8.4±14.4 weeks. Many cases required neurosurgical intervention (47.2%), including open biopsy (41.4%), decompression (28.1%), and fixation (26.9%).
Inflammatory markers normalized in 39.8% of cases (ESR in 13.7%, CRP in 34.2%). After discharge, 31.9% of patients were re-admitted within 90 days. The 1-year mortality rate was 8.4%; of the survivors at 1-year, 26.6% had a neurologic deficit and 4.6% had a bowel/bladder deficit.
Factors significantly associated with 1-year mortality included age (p=0.010), failure to complete the prescribed antibiotic course (p=0.015), concomitant infection (p=0.005), failure of CRP normalization (p=0.038), and final actual CRP level (p=0.001). Need for surgery was not associated with 1-year mortality.
Conclusion : Spondylodiscitis can carry a high 1-year mortality rate. Patient age and concurrent infections are associated with mortality, as is failure to complete prescribed medical therapy. CRP may be a more significant predictor of mortality than ESR.
