No-Reflow in Acute Ischemic Stroke: Measurement, Mechanisms and Molecular Markers
No-reflow in Acute Ischemic Stroke: Measurement, Mechanisms and Molecular Markers
Friday, April 21, 2023

Colin P. Sperring, BS
Medical Student
Columbia University Vagelos College of Physicians and Surgeons
New York, New York, United States
ePoster Presenter(s)
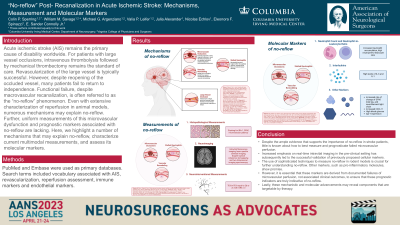
Introduction: Acute ischemic stroke (AIS) remains the primary cause of disability worldwide. Among patients with AIS due to large vessel occlusion (LVO), mechanical thrombectomy (MT) yields >80% recanalization rates. However, the majority of these patients still do not return to an independent life. Impaired microvascular reperfusion, often referred to as “no-reflow”, may contribute to poor outcomes despite macrovascular recanalization. However, despite extensive characterization of reperfusion in animal models, uniform measurements of microvascular dysfunction and prognostic markers associated with no-reflow are lacking. We set out to characterize current measurements of no-reflow in AIS as well as associated molecular markers and mechanisms.
Methods: PubMed and Embase were used as primary databases. Search terms included vocabulary associated with AIS, revascularization, reperfusion assessment, immune markers and endothelial markers.
Results: Over 2000 studies were screened. 33 studies met our criteria, including 12 clinical and 21 preclinical studies. Clinical studies assessed no-reflow using a wide-array of measurements, including cerebral blood volume (CBV) and cerebral blood flow (CBF) mapping, the Thrombolysis in Cerebral Infarction scale, and the modified Rankin Scale. Preclinical studies characterized no-reflow with a similarly large variety of measurements, including in vivo microscopy, immunohistochemistry, radiography, and macro- and micro-vascular CBF and CBV. Clinical studies reported a number of inflammatory markers associated with no-reflow, including peripheral neutrophil-lymphocyte-ratio, IL-6, and CXCL-11. Pre-clinical studies implicated key genes in no-reflow, including LFA-1, CD40, P-selectin, as well as cellular events, such as pericyte contraction and leukocyte adhesion.
Conclusion : Together, these studies suggest a number of inflammatory markers that could be measured within the clinic to assess impaired microvascular reperfusion in AIS patients. Further, they identify key molecular pathways that could inform future therapeutic targeting. However, there is still no consistent method of measuring or defining the no-reflow phenomenon in AIS.
Methods: PubMed and Embase were used as primary databases. Search terms included vocabulary associated with AIS, revascularization, reperfusion assessment, immune markers and endothelial markers.
Results: Over 2000 studies were screened. 33 studies met our criteria, including 12 clinical and 21 preclinical studies. Clinical studies assessed no-reflow using a wide-array of measurements, including cerebral blood volume (CBV) and cerebral blood flow (CBF) mapping, the Thrombolysis in Cerebral Infarction scale, and the modified Rankin Scale. Preclinical studies characterized no-reflow with a similarly large variety of measurements, including in vivo microscopy, immunohistochemistry, radiography, and macro- and micro-vascular CBF and CBV. Clinical studies reported a number of inflammatory markers associated with no-reflow, including peripheral neutrophil-lymphocyte-ratio, IL-6, and CXCL-11. Pre-clinical studies implicated key genes in no-reflow, including LFA-1, CD40, P-selectin, as well as cellular events, such as pericyte contraction and leukocyte adhesion.
Conclusion : Together, these studies suggest a number of inflammatory markers that could be measured within the clinic to assess impaired microvascular reperfusion in AIS patients. Further, they identify key molecular pathways that could inform future therapeutic targeting. However, there is still no consistent method of measuring or defining the no-reflow phenomenon in AIS.
