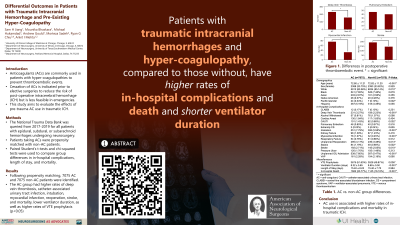
Patterns of Care in Patients with Traumatic Intracranial Hemorrhage and Pre-Existing Hypercoagulopathy
Patterns of Care in Patients with Traumatic Intracranial Hemorrhage and Pre-existing Hypercoagulopathy
Friday, April 21, 2023
Sam H. Jiang, BS (he/him/his)
Medical Student
University of Illinois College of Medicine at Chicago
Chicago, Illinois, United States
ePoster Presenter(s)
Introduction: Anticoagulants (ACs) are often prescribed on a daily basis in patients with hypercoagulopathies to prevent thromboembolic events. While cessation of ACs is indicated prior to elective surgeries to reduce the risk of post-operative intracerebral hemorrhage (ICH), it is not feasible in patients undergoing emergent surgery for traumatic ICH. Thus, a comprehensive understanding of the post-operative complications associated with pre-trauma AC use is warranted to guide patient care in an acute setting.
Methods: The National Trauma Data Bank was queried from 2017-2019 for all patients with epidural, subdural, or subarachnoid hemorrhages subsequently undergoing neurosurgical intervention. Patients taking anticoagulants, antiplatelet therapy, thrombin inhibitors, or thrombolytic agents (AC) were propensity matched with patients not on anticoagulant medications (non-AC) based on demographics, comorbidities, type of hemorrhage, and venous thromboembolism (VTE) prophylaxis. Paired Student’s t-tests and chi-squared tests were used to compare differences in in-hospital complications, length of stay, and rate of mortality between the two groups (α=0.05)
Results: Following 1-to-1 propensity matching, 7075 AC patients and 7075 non-AC patients were identified. The AC group had higher rates of deep vein thrombosis, catheter-associated urinary tract infection, intubation, myocardial infarction, reoperation, stroke, and mortality, but lower ventilator duration (p < 0.05). The AC group also had higher rates of VTE prophylaxis, however the rates were comparable (AC=51.63%, non-AC=49.87%, p=0.036).
Conclusion : In patients with traumatic ICH undergoing neurosurgical intervention, pre-trauma AC use is associated with higher rates of in-hospital complications and mortality. Further research is warranted to examine the timing and use of reversal agents for ACs as well as increased monitoring for delayed ICHs. Understanding these risks will help providers adopt effective clinical practices to manage patients that are susceptible to poor outcomes in the setting of blunt and acute trauma.
Methods: The National Trauma Data Bank was queried from 2017-2019 for all patients with epidural, subdural, or subarachnoid hemorrhages subsequently undergoing neurosurgical intervention. Patients taking anticoagulants, antiplatelet therapy, thrombin inhibitors, or thrombolytic agents (AC) were propensity matched with patients not on anticoagulant medications (non-AC) based on demographics, comorbidities, type of hemorrhage, and venous thromboembolism (VTE) prophylaxis. Paired Student’s t-tests and chi-squared tests were used to compare differences in in-hospital complications, length of stay, and rate of mortality between the two groups (α=0.05)
Results: Following 1-to-1 propensity matching, 7075 AC patients and 7075 non-AC patients were identified. The AC group had higher rates of deep vein thrombosis, catheter-associated urinary tract infection, intubation, myocardial infarction, reoperation, stroke, and mortality, but lower ventilator duration (p < 0.05). The AC group also had higher rates of VTE prophylaxis, however the rates were comparable (AC=51.63%, non-AC=49.87%, p=0.036).
Conclusion : In patients with traumatic ICH undergoing neurosurgical intervention, pre-trauma AC use is associated with higher rates of in-hospital complications and mortality. Further research is warranted to examine the timing and use of reversal agents for ACs as well as increased monitoring for delayed ICHs. Understanding these risks will help providers adopt effective clinical practices to manage patients that are susceptible to poor outcomes in the setting of blunt and acute trauma.
