eVisit use in Neurosurgery – Trends in Use and Access to Care
Evisit Use in Neurosurgery – Trends in Use and Access to Care
Friday, April 21, 2023

Maya Harary, MD
Resident
University of California, Los Angeles
Los Angeles, California, United States
ePoster Presenter(s)
Introduction: The COVID pandemic lead to an overnight adoption of telemedicine throughout the medical field, including neurosurgery. Little is known regarding the long-term sustainment of this trend, nor about whether all patients are equally likely to adopt, and potentially benefit from, remote care via telemedicine.
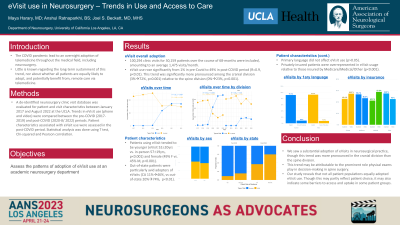
Methods: A de-identified neurosurgery clinic visit database was evaluated for patient and visit characteristics between January 2017 and August 2022 at the UCLA. Trends in eVisit use (phone and video) were compared between the pre-COVID (2017-2019) and post-COVID (2020-8/ 2022) periods. Patient characteristics associated with eVisit use were assessed in the post-COVID period. Statistical analysis was done using T test, Chi-squared and Pearson correlation.
Results: 100,294 clinic visits for 30,159 patients over the course of 68-months were included, amounting to an average 1,475 visits/month. eVisit use rose significantly from 1% in pre-Covid to 49% in post-COVID period (R=0.9, p< 0.01). This trend was significantly more pronounced among the cranial division (3%->72%, p< 0.001) relative to the spine division (0%->23%, p< 0.001). Patients using eVisit tended to be younger (eVisit 52+/-20yrs vs. in-person 57+/-19yrs, p< 0.001) and female (49% F vs. 45% M, p< 0.001). Out-of-state patients were particularly avid adopters of eVisits (CA 11%->46%, vs out-of-state 20%->4%, p< 0.01). Primary language did not affect eVisit use (p>0.05). Privately insured patients were overrepresented in eVisit usage relative to those insured by Medicare/Medical/Other (p < 0.001).
Conclusion : We confirm the substantial adoption of eVisits in neurosurgical practice, though this trend was more pronounced in the cranial division than the spine division. This may be attributable to the prominent role physical exams play in decision-making in spine surgery. Our study reveals that not all patient populations equally adopted eVisit use. Though this may partly reflect patient choice, it may also indicate some barriers to access and uptake in some patient groups.
Methods: A de-identified neurosurgery clinic visit database was evaluated for patient and visit characteristics between January 2017 and August 2022 at the UCLA. Trends in eVisit use (phone and video) were compared between the pre-COVID (2017-2019) and post-COVID (2020-8/ 2022) periods. Patient characteristics associated with eVisit use were assessed in the post-COVID period. Statistical analysis was done using T test, Chi-squared and Pearson correlation.
Results: 100,294 clinic visits for 30,159 patients over the course of 68-months were included, amounting to an average 1,475 visits/month. eVisit use rose significantly from 1% in pre-Covid to 49% in post-COVID period (R=0.9, p< 0.01). This trend was significantly more pronounced among the cranial division (3%->72%, p< 0.001) relative to the spine division (0%->23%, p< 0.001). Patients using eVisit tended to be younger (eVisit 52+/-20yrs vs. in-person 57+/-19yrs, p< 0.001) and female (49% F vs. 45% M, p< 0.001). Out-of-state patients were particularly avid adopters of eVisits (CA 11%->46%, vs out-of-state 20%->4%, p< 0.01). Primary language did not affect eVisit use (p>0.05). Privately insured patients were overrepresented in eVisit usage relative to those insured by Medicare/Medical/Other (p < 0.001).
Conclusion : We confirm the substantial adoption of eVisits in neurosurgical practice, though this trend was more pronounced in the cranial division than the spine division. This may be attributable to the prominent role physical exams play in decision-making in spine surgery. Our study reveals that not all patient populations equally adopted eVisit use. Though this may partly reflect patient choice, it may also indicate some barriers to access and uptake in some patient groups.
