Minimizing intracranial disease prior to stereotactic radiation in single or solitary brain metastases
Minimizing Intracranial Disease Prior to Stereotactic Radiation in Single or Solitary Brain Metastases
Friday, April 21, 2023
Wenya Linda Bi, MD, PhD
Neurosurgeon
Brigham & Women's Hospital
Boston, Massachusetts, United States
ePoster Presenter(s)
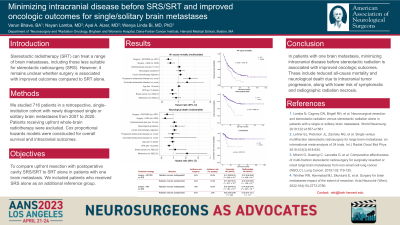
Introduction: The optimal application of neurosurgical resection and brain-directed radiation to treating brain metastases has evolved as newer systemic therapies have improved extracranial disease control. Stereotactic radiotherapy (SRT) has proved effective in a wide range of brain metastases, including those less suitable for single-fraction stereotactic radiosurgery (SRS). However, previous studies have shown equivocal results regarding whether surgery correlates with improved outcomes compared to SRT alone. We compared resection with cavity SRT/SRS to SRT alone in patients with one newly diagnosed brain metastasis.
Methods: We studied 747 patients in a retrospective, single-institution cohort diagnosed with a single or solitary brain metastasis from 2007 to 2020. Cox regression models were constructed for all-cause mortality, local recurrence, and additional intracranial outcomes.
Results: Surgery with cavity SRT/SRS was associated with prolonged overall survival compared to SRT alone. This effect remained significant after adjustment for relevant factors at the time of brain metastasis diagnosis, including patient age, performance status, unidimensional tumor size, presence of neurological symptoms, presence and progression status of extracranial disease, and number of previous chemotherapy regimens for metastatic disease (HR for surgery + SRT: 0.48, 95% CI [0.34-0.69], p=6.03E-05; HR for surgery + SRS: 0.52, 95% CI [0.34-0.81], p=3.55E-03). When compared with SRT alone in multivariable models, resection with SRS was associated with lower risk of neurological death attributable to intracranial tumor progression (HR: 0.33, 95% CI [0.13-0.81], p=1.64E-02) while resection with SRT was associated with longer time to local recurrence (HR: 0.36, 95% CI [0.16-0.81], p=1.45E-02). Among surgical patients, gross total resection was associated with prolonged overall survival (HR: 0.66, 95% CI [0.44-0.98], p=3.85E-02) and lower risk of local recurrence (HR: 0.34, 95% CI [0.17-0.69], p=2.74E-03).
Conclusion : In patients with one brain metastasis, minimizing intracranial disease specifically prior to stereotactic radiation is associated with prolonged overall survival and local recurrence-free survival.
Methods: We studied 747 patients in a retrospective, single-institution cohort diagnosed with a single or solitary brain metastasis from 2007 to 2020. Cox regression models were constructed for all-cause mortality, local recurrence, and additional intracranial outcomes.
Results: Surgery with cavity SRT/SRS was associated with prolonged overall survival compared to SRT alone. This effect remained significant after adjustment for relevant factors at the time of brain metastasis diagnosis, including patient age, performance status, unidimensional tumor size, presence of neurological symptoms, presence and progression status of extracranial disease, and number of previous chemotherapy regimens for metastatic disease (HR for surgery + SRT: 0.48, 95% CI [0.34-0.69], p=6.03E-05; HR for surgery + SRS: 0.52, 95% CI [0.34-0.81], p=3.55E-03). When compared with SRT alone in multivariable models, resection with SRS was associated with lower risk of neurological death attributable to intracranial tumor progression (HR: 0.33, 95% CI [0.13-0.81], p=1.64E-02) while resection with SRT was associated with longer time to local recurrence (HR: 0.36, 95% CI [0.16-0.81], p=1.45E-02). Among surgical patients, gross total resection was associated with prolonged overall survival (HR: 0.66, 95% CI [0.44-0.98], p=3.85E-02) and lower risk of local recurrence (HR: 0.34, 95% CI [0.17-0.69], p=2.74E-03).
Conclusion : In patients with one brain metastasis, minimizing intracranial disease specifically prior to stereotactic radiation is associated with prolonged overall survival and local recurrence-free survival.
