The obesity paradox does not apply to patients undergoing mechanical thrombectomy: Institutional experience and meta-analysis
The Obesity Paradox Does Not Apply to Patients Undergoing Mechanical Thrombectomy: Institutional Experience and Meta-analysis
Friday, April 21, 2023

Haydn Hoffman, MD
Resident
SUNY Upstate
Syracuse, New York, United States
ePoster Presenter(s)
Introduction: Previous studies have supported the presence of an obesity paradox in vascular diseases, whereby patients with higher body mass index (BMI) experience improved outcomes. There is conflicting evidence regarding whether this applies to patients undergoing mechanical thrombectomy (MT) for large vessel occlusion (LVO).
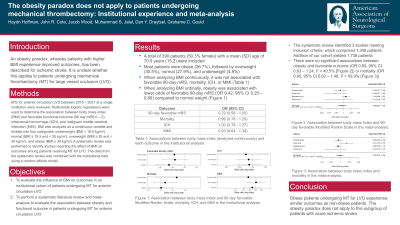
Methods: All MTs for anterior circulation LVO between 2015 – 2021 at a single institution were reviewed. Multivariate logistic regression analysis adjusting for age, comorbidities, premorbid mRS, admission NIHSS, ASPECTS, collateral score, tPA administration, onset to reperfusion time, and TICI was used to determine the association between BMI and favorable functional outcome (mRS 0 – 2 at 90 days). In addition, a systematic review of the literature was performed to identify studies reporting the effect of BMI on outcomes among patients receiving MT for LVO. The data from the systematic review was combined with the institutional data using a random effects model.
Results: In the institutional cohort there were 390 patients (50.3% female) with a mean (SD) age of 70.9 years (15.2). There were 143 (36.7%) obese (BMI >= 30 kg/m2) and 247 (63.3%) non-obese (BMI < 30 kg/m2) patients, and the proportions of favorable functional outcomes were 30.1% and 35.2%, respectively. In the multivariate analysis, obesity was associated with lower odds of favorable functional outcome (OR 0.49, 95% CI 0.27 – 0.89) compared to non-obesity. The systematic review identified 3 eligible studies comprising 1,237 patients for a total of 1,627 patients. In the meta-analysis, the proportion of patients experiencing a favorable outcome in the obese and non-obese groups were 37.9% and 38%, respectively. In the random effects model there was no significant association between obesity and favorable outcome (OR 0.89, 95% CI 0.63 – 1.24).
Conclusion : Obesity is not associated with favorable functional outcomes in patients undergoing MT for LVO.
Methods: All MTs for anterior circulation LVO between 2015 – 2021 at a single institution were reviewed. Multivariate logistic regression analysis adjusting for age, comorbidities, premorbid mRS, admission NIHSS, ASPECTS, collateral score, tPA administration, onset to reperfusion time, and TICI was used to determine the association between BMI and favorable functional outcome (mRS 0 – 2 at 90 days). In addition, a systematic review of the literature was performed to identify studies reporting the effect of BMI on outcomes among patients receiving MT for LVO. The data from the systematic review was combined with the institutional data using a random effects model.
Results: In the institutional cohort there were 390 patients (50.3% female) with a mean (SD) age of 70.9 years (15.2). There were 143 (36.7%) obese (BMI >= 30 kg/m2) and 247 (63.3%) non-obese (BMI < 30 kg/m2) patients, and the proportions of favorable functional outcomes were 30.1% and 35.2%, respectively. In the multivariate analysis, obesity was associated with lower odds of favorable functional outcome (OR 0.49, 95% CI 0.27 – 0.89) compared to non-obesity. The systematic review identified 3 eligible studies comprising 1,237 patients for a total of 1,627 patients. In the meta-analysis, the proportion of patients experiencing a favorable outcome in the obese and non-obese groups were 37.9% and 38%, respectively. In the random effects model there was no significant association between obesity and favorable outcome (OR 0.89, 95% CI 0.63 – 1.24).
Conclusion : Obesity is not associated with favorable functional outcomes in patients undergoing MT for LVO.
