Characteristics and Inpatient Outcomes of Patients Selected for Surgical Treatment of Trigeminal Neuralgia
Friday, April 21, 2023

Ariel Sacknovitz, MS
Medical Student
New York Medical College
Flushing, New York, United States
ePoster Presenter(s)
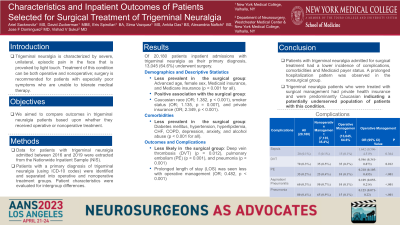
Introduction: Trigeminal neuralgia is characterized by severe, unilateral, episodic pain in the face that is provoked by light touch. Treatment of this condition can be both operative and nonoperative; surgery is recommended for patients with especially poor symptoms who are unable to tolerate medical therapy. We aimed to compare outcomes in trigeminal neuralgia patients based upon whether they received operative or nonoperative treatment.
Methods: Data for patients with trigeminal neuralgia admitted between 2016 and 2019 were extracted from the Nationwide Inpatient Sample. We identified patients with a primary diagnosis of trigeminal neuralgia (using ICD-10 codes) and separated them into operative and nonoperative treatment groups. Patient characteristics were evaluated for intergroup differences.
Results: Of 20,180 patients inpatient admissions with trigeminal neuralgia, 13,045 (64.6%) underwent surgery. Advanced age, female sex, Medicaid insurance, and Medicare insurance were less prevalent in the surgical group (p < 0.001 for all). Factors positively associated with surgical treatment were Caucasian race (OR; 1.382, p < 0.001), smoker status (OR; 1.135, p = 0.007), and private insurance (OR; 2.349, p < 0.001). Diabetes mellitus, hypertension, hyperlipidemia, CHF, COPD, depression, anxiety, and alcohol abuse were also less prevalent in the surgical cohort (p < 0.001 for all). The surgery group was less likely to have had deep vein thrombosis (p = 0.012), pulmonary embolism (p < 0.001), or pneumonia (p < 0.001). Prolonged length of stay was seen less with operative management (OR; 0.482, p < 0.001).
Conclusion : Patients with trigeminal neuralgia admitted for surgical treatment had a lower incidence of complications, comorbidities and Medicaid payer status. A prolonged hospitalization pattern was observed in the nonsurgical group. Our findings also indicate that trigeminal neuralgia patients who were treated with surgical management had private health insurance and were predominantly Caucasian, indicating a potentially underserved population of patients with this condition.
Methods: Data for patients with trigeminal neuralgia admitted between 2016 and 2019 were extracted from the Nationwide Inpatient Sample. We identified patients with a primary diagnosis of trigeminal neuralgia (using ICD-10 codes) and separated them into operative and nonoperative treatment groups. Patient characteristics were evaluated for intergroup differences.
Results: Of 20,180 patients inpatient admissions with trigeminal neuralgia, 13,045 (64.6%) underwent surgery. Advanced age, female sex, Medicaid insurance, and Medicare insurance were less prevalent in the surgical group (p < 0.001 for all). Factors positively associated with surgical treatment were Caucasian race (OR; 1.382, p < 0.001), smoker status (OR; 1.135, p = 0.007), and private insurance (OR; 2.349, p < 0.001). Diabetes mellitus, hypertension, hyperlipidemia, CHF, COPD, depression, anxiety, and alcohol abuse were also less prevalent in the surgical cohort (p < 0.001 for all). The surgery group was less likely to have had deep vein thrombosis (p = 0.012), pulmonary embolism (p < 0.001), or pneumonia (p < 0.001). Prolonged length of stay was seen less with operative management (OR; 0.482, p < 0.001).
Conclusion : Patients with trigeminal neuralgia admitted for surgical treatment had a lower incidence of complications, comorbidities and Medicaid payer status. A prolonged hospitalization pattern was observed in the nonsurgical group. Our findings also indicate that trigeminal neuralgia patients who were treated with surgical management had private health insurance and were predominantly Caucasian, indicating a potentially underserved population of patients with this condition.
