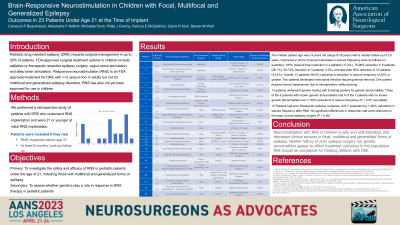
Brain-Responsive Neurostimulation in Children – Outcomes in 25 Patients Under Age 21 at the Time of Implant
Brain-responsive Neurostimulation in Children – Outcomes in 25 Patients Under Age 21 at the Time of Implant
Friday, April 21, 2023

Cameron P. Beaudreault, MS
Medical Student
New York Medical College
Valhalla, New York, United States
ePoster Presenter(s)
Introduction: Pediatric drug resistant epilepsy (DRE) requires surgical management in up to 30% of patients. FDA-approved surgical treatment options in children include palliative or therapeutic resective epilepsy surgery, vagus nerve stimulation and deep brain stimulation. Responsive neurostimulation (RNS) is an FDA approved treatment for DRE with = < 2 seizure foci in adults but has not yet been approved for use in children. Genetic testing may help identify ideal candidates for this surgical intervention.
Methods: We performed a retrospective study of 25 patients with DRE who underwent RNS implantation in our practice and were 21 or younger at initial RNS implantation.
Results: The median patient age was 15 years old (range 9-18 years) with median follow-up of 26 months. Outcomes in terms of percent decrease in seizure frequency were as follows (in quartiles): 100% (seizure free) reduction in 5 patients (20%), 75-99% reduction in 6 patients (24%), 50-74% reduction in 3 patients (12%), and less than 50% reduction in 11 patients (44%). Overall, 14 patients (56%) achieved a reduction in seizure frequency of 50% or greater. Two patients developed intracranial infection requiring device removal. One patient required device replacement due to intraoperative malfunctioning.
A sub-cohort of 15 patients underwent genetic testing, 6 of these testing positive for genetic abnormalities. Three of the 6 patients with genetic abnormalities had >= 50% reductions in seizure frequency, and 3 patients with negative results for genetic abnormalities achieved seizure freedom.
Conclusion : Neuromodulation with RNS in children is safe, well-tolerated, and decreases clinical seizures in multiple forms of DRE. History of prior epilepsy surgery and genetic abnormalities do not appear to affect treatment outcomes in this population.
Methods: We performed a retrospective study of 25 patients with DRE who underwent RNS implantation in our practice and were 21 or younger at initial RNS implantation.
Results: The median patient age was 15 years old (range 9-18 years) with median follow-up of 26 months. Outcomes in terms of percent decrease in seizure frequency were as follows (in quartiles): 100% (seizure free) reduction in 5 patients (20%), 75-99% reduction in 6 patients (24%), 50-74% reduction in 3 patients (12%), and less than 50% reduction in 11 patients (44%). Overall, 14 patients (56%) achieved a reduction in seizure frequency of 50% or greater. Two patients developed intracranial infection requiring device removal. One patient required device replacement due to intraoperative malfunctioning.
A sub-cohort of 15 patients underwent genetic testing, 6 of these testing positive for genetic abnormalities. Three of the 6 patients with genetic abnormalities had >= 50% reductions in seizure frequency, and 3 patients with negative results for genetic abnormalities achieved seizure freedom.
Conclusion : Neuromodulation with RNS in children is safe, well-tolerated, and decreases clinical seizures in multiple forms of DRE. History of prior epilepsy surgery and genetic abnormalities do not appear to affect treatment outcomes in this population.
