Are there Racial Disparities in Resource Utilization After Surgery for Metastatic Spinal Column Tumors?
Are There Racial Disparities in Resource Utilization After Surgery for Metastatic Spinal Column Tumors?
Friday, April 21, 2023

Aladine A. Elsamadicy, MD
Resident Physician
Yale School of Medicine
New Haven, Connecticut, United States
ePoster Presenter(s)
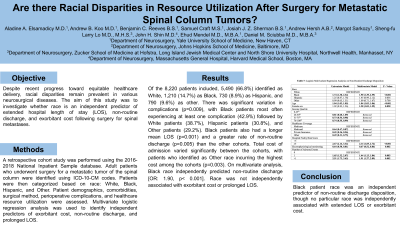
Introduction: Despite recent progress toward equitable healthcare delivery, racial disparities remain prevalent in various neurosurgical diseases. The aim of this study was to investigate whether race is an independent predictor of extended hospital length of stay (LOS), non-routine discharge, and exorbitant cost following surgery for spinal metastases.
Methods: A retrospective cohort study was performed using the 2016-2018 National Inpatient Sample database. Adult patients who underwent surgery for a metastatic tumor of the spinal column were identified using ICD-10-CM codes. Patients were then categorized based on race: White, Black, Hispanic, and Other. Patient demographics, comorbidities, surgical method, perioperative complications, and healthcare resource utilization were assessed. Multivariate logistic regression analysis was used to identify independent predictors of exorbitant cost, non-routine discharge, and prolonged LOS.
Results: Of the 8,220 patients included, 5,490 (66.8%) identified as White, 1,210 (14.7%) as Black, 730 (8.9%) as Hispanic, and 790 (9.6%) as other. There was significant variation in complications (p=0.009), with Black patients most often experiencing at least one complication (42.9%) followed by White patients (38.7%), Hispanic patients (30.8%), and Other patients (29.2%). Black patients also had a longer mean LOS (p=0.001) and a greater rate of non-routine discharge (p=0.005) than the other cohorts. Total cost of admission varied significantly between the cohorts, with patients who identified as Other race incurring the highest cost among the cohorts (p=0.003). On multivariate analysis, Black race independently predicted non-routine discharge [OR: 1.90, p< 0.001]. Race was not independently associated with exorbitant cost or prolonged LOS.
Conclusion : Black race was an independent predictor of non-routine discharge disposition, though no particular race was independently associated with extended LOS or exorbitant cost. Further studies that determine why these disparities exist may lead to interventions that increase the quality of spinal tumor treatment and reduce soaring healthcare costs.
Methods: A retrospective cohort study was performed using the 2016-2018 National Inpatient Sample database. Adult patients who underwent surgery for a metastatic tumor of the spinal column were identified using ICD-10-CM codes. Patients were then categorized based on race: White, Black, Hispanic, and Other. Patient demographics, comorbidities, surgical method, perioperative complications, and healthcare resource utilization were assessed. Multivariate logistic regression analysis was used to identify independent predictors of exorbitant cost, non-routine discharge, and prolonged LOS.
Results: Of the 8,220 patients included, 5,490 (66.8%) identified as White, 1,210 (14.7%) as Black, 730 (8.9%) as Hispanic, and 790 (9.6%) as other. There was significant variation in complications (p=0.009), with Black patients most often experiencing at least one complication (42.9%) followed by White patients (38.7%), Hispanic patients (30.8%), and Other patients (29.2%). Black patients also had a longer mean LOS (p=0.001) and a greater rate of non-routine discharge (p=0.005) than the other cohorts. Total cost of admission varied significantly between the cohorts, with patients who identified as Other race incurring the highest cost among the cohorts (p=0.003). On multivariate analysis, Black race independently predicted non-routine discharge [OR: 1.90, p< 0.001]. Race was not independently associated with exorbitant cost or prolonged LOS.
Conclusion : Black race was an independent predictor of non-routine discharge disposition, though no particular race was independently associated with extended LOS or exorbitant cost. Further studies that determine why these disparities exist may lead to interventions that increase the quality of spinal tumor treatment and reduce soaring healthcare costs.
