Prevalence and Influence of Frailty on Hospital Outcomes after Surgical Resection for Benign and Malignant Spinal Meningiomas
Prevalence and Influence of Frailty on Hospital Outcomes After Surgical Resection for Benign and Malignant Spinal Meningiomas
Friday, April 21, 2023

Aladine A. Elsamadicy, MD
Resident Physician
Yale School of Medicine
New Haven, Connecticut, United States
ePoster Presenter(s)
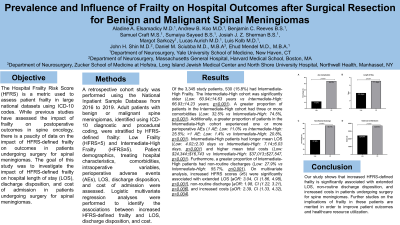
Introduction: The Hospital Frailty Risk Score (HFRS) is a metric used to assess patient frailty in large national datasets. While previous studies have assessed the impact of frailty on postoperative outcomes in spine oncology, there are few studies discussing the impact of HFRS-defined frailty on outcomes in patients undergoing surgery for spinal meningiomas. The goal of this study was to investigate the impact of HFRS-defined frailty on hospital length of stay (LOS), discharge disposition, and costs in patients undergoing surgery for spinal meningiomas.
Methods: A retrospective cohort study was performed using the National Inpatient Sample Database (2016-2019). Adult patients with benign or malignant spine meningiomas, identified using ICD-10 coding, were stratified by HFRS-defined frailty: Low Frailty (HFRS < 5) and Intermediate-High (IH) Frailty (HFRS≥5). Demographics, treating hospital characteristics, comorbidities, intraoperative variables, adverse events (AEs), LOS, discharge disposition, and costs were assessed. Multivariate analyses identified the associations between increased HFRS-defined frailty and LOS, discharge disposition, and costs.
Results: Of the 3,345 study patients, 530 (15.8%) had IH Frailty. The IH cohort was significantly older (p < 0.001) and had a greater proportion of patients with ≥3 comorbidities (p < 0.001). Additionally, a greater proportion of patients in the IH cohort experienced ≥1 perioperative AE (1 AE: Low: 11.0% vs IH: 25.5%; >1 AE: Low: 1.4% vs IH: 20.8%,p < 0.001). IH patients had longer mean LOS (Low: 4.02±2.30 days vs IH: 7.14±6.03 days,p < 0.001), higher mean total costs (Low: $24,344±$16,743 vs IH: $37,013±$27,547,p < 0.001), and greater rates of non-routine discharge (Low: 27.9% vs IH: 55.7%,p < 0.001). On multivariate analysis, increased HFRS scores (≥5) were significantly associated with extended LOS [aOR:3.04,p < 0.001], non-routine discharge [aOR:1.98,p=0.006], and increased costs [aOR:2.39,p=0.004].
Conclusion : Our study shows that increased HFRS-defined frailty is significantly associated with extended LOS, non-routine discharge disposition, and increased costs in patients undergoing surgery for spine meningiomas.
Methods: A retrospective cohort study was performed using the National Inpatient Sample Database (2016-2019). Adult patients with benign or malignant spine meningiomas, identified using ICD-10 coding, were stratified by HFRS-defined frailty: Low Frailty (HFRS < 5) and Intermediate-High (IH) Frailty (HFRS≥5). Demographics, treating hospital characteristics, comorbidities, intraoperative variables, adverse events (AEs), LOS, discharge disposition, and costs were assessed. Multivariate analyses identified the associations between increased HFRS-defined frailty and LOS, discharge disposition, and costs.
Results: Of the 3,345 study patients, 530 (15.8%) had IH Frailty. The IH cohort was significantly older (p < 0.001) and had a greater proportion of patients with ≥3 comorbidities (p < 0.001). Additionally, a greater proportion of patients in the IH cohort experienced ≥1 perioperative AE (1 AE: Low: 11.0% vs IH: 25.5%; >1 AE: Low: 1.4% vs IH: 20.8%,p < 0.001). IH patients had longer mean LOS (Low: 4.02±2.30 days vs IH: 7.14±6.03 days,p < 0.001), higher mean total costs (Low: $24,344±$16,743 vs IH: $37,013±$27,547,p < 0.001), and greater rates of non-routine discharge (Low: 27.9% vs IH: 55.7%,p < 0.001). On multivariate analysis, increased HFRS scores (≥5) were significantly associated with extended LOS [aOR:3.04,p < 0.001], non-routine discharge [aOR:1.98,p=0.006], and increased costs [aOR:2.39,p=0.004].
Conclusion : Our study shows that increased HFRS-defined frailty is significantly associated with extended LOS, non-routine discharge disposition, and increased costs in patients undergoing surgery for spine meningiomas.
