Does Low Grade vs. High Grade Bilsky Score Influence Local Recurrence and Overall Survival in Metastatic Spine Tumor Surgery?
Friday, April 21, 2023

Scott L. Zuckerman, MD, MPH
Assistant Professor of Neurosurgery and Orthopaedics
Vanderbilt University Medical Center
Nashville, Tennessee, United States
ePoster Presenter(s)
Introduction: Spinal cord compression caused by spinal tumors is measured using the epidural spinal cord compression scale (ESCC), also known as the Bilsky score. Whether Bilsky score affects short/long-term outcomes remains unknown. We sought to compare the impact of Bilsky score 0-1 vs. 2-3 with regards to: 1) preoperative presentation, 2) perioperative variables, and 3) long-term outcomes.
Methods: A single-center, retrospective cohort study was undertaken of patients undergoing metastatic spine surgery between 01/2010-01/2021. Multivariate logistic/linear/Cox regression were performed, controlling for age, BMI, race, total decompressed levels, tumor size, other organ metastasis, and postoperative radiotherapy/chemotherapy.
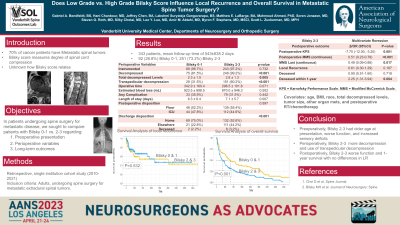
Results: Of 343 patients with extradural spinal metastasis, 92(26.8%) patients presented with Bilsky 0-1 and 251(73.2%) with Bilsky 2-3. Preoperatively: Patients with Bilsky 2-3 were older(p=0.008), presented more frequently with sensory deficits(p=0.029), and had worse preoperative Karnofsky Performance Score(KPS)(p=0.002). Perioperatively: Preoperative/postoperative chemotherapy and radiotherapy were similar between the two groups. However, patients with Bilsky 2-3 had more total decompressed levels(p=0.005) and more transpedicular decompression(p < 0.001), with similar operative time(p=0.071) and EBL(p=0.502), complication rates(p=0.442), and neurological deficit(p=0.852) compared to Bilsky 0-1. Interestingly, patients with Bilsky 2-3 had a longer length of stay(LOS)(p=0.007) with less home discharge(p < 0.001). Long-term: No difference was found in 90-day readmissions(p=0.607), reoperation(p=0.510), LR(p=0.100), and time to LR(log-rank;p=0.532). However, patients with Bilsky 2-3 had significantly worse postoperative KPS(p < 0.001), worse Modified McCormick Scale (MMS)(p=0.003), shorter OS(log-rank;p < 0.001), and worse 1-year survival (p=0.012). Bilsky 2-3 lesions were also associated with shorter OS on univariate and multivariate Cox regression(HR=1.78,95%CI=1.27-2.49,p < 0.001), with no significant impact on time to LR.
Conclusion : Bilsky 2-3 lesions were associated with longer LOS, more non-home discharge, worse postoperative KPS/MMS, shorter OS, and reduced survival at one year, compared to Bilsky 0-1, with no significant difference in short-term outcomes or LR. Higher grade Bilsky score lesions are at a higher risk for worse outcomes, including decreased survival.
Methods: A single-center, retrospective cohort study was undertaken of patients undergoing metastatic spine surgery between 01/2010-01/2021. Multivariate logistic/linear/Cox regression were performed, controlling for age, BMI, race, total decompressed levels, tumor size, other organ metastasis, and postoperative radiotherapy/chemotherapy.
Results: Of 343 patients with extradural spinal metastasis, 92(26.8%) patients presented with Bilsky 0-1 and 251(73.2%) with Bilsky 2-3. Preoperatively: Patients with Bilsky 2-3 were older(p=0.008), presented more frequently with sensory deficits(p=0.029), and had worse preoperative Karnofsky Performance Score(KPS)(p=0.002). Perioperatively: Preoperative/postoperative chemotherapy and radiotherapy were similar between the two groups. However, patients with Bilsky 2-3 had more total decompressed levels(p=0.005) and more transpedicular decompression(p < 0.001), with similar operative time(p=0.071) and EBL(p=0.502), complication rates(p=0.442), and neurological deficit(p=0.852) compared to Bilsky 0-1. Interestingly, patients with Bilsky 2-3 had a longer length of stay(LOS)(p=0.007) with less home discharge(p < 0.001). Long-term: No difference was found in 90-day readmissions(p=0.607), reoperation(p=0.510), LR(p=0.100), and time to LR(log-rank;p=0.532). However, patients with Bilsky 2-3 had significantly worse postoperative KPS(p < 0.001), worse Modified McCormick Scale (MMS)(p=0.003), shorter OS(log-rank;p < 0.001), and worse 1-year survival (p=0.012). Bilsky 2-3 lesions were also associated with shorter OS on univariate and multivariate Cox regression(HR=1.78,95%CI=1.27-2.49,p < 0.001), with no significant impact on time to LR.
Conclusion : Bilsky 2-3 lesions were associated with longer LOS, more non-home discharge, worse postoperative KPS/MMS, shorter OS, and reduced survival at one year, compared to Bilsky 0-1, with no significant difference in short-term outcomes or LR. Higher grade Bilsky score lesions are at a higher risk for worse outcomes, including decreased survival.
