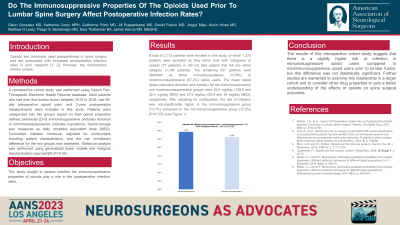
Do The Immunosuppressive Properties of Opioid Used Prior to Lumbar Spine Surgery Affect Postoperative Infection Rates?
Do the Immunosuppressive Properties of Opioid Used Prior to Lumbar Spine Surgery Affect Postoperative Infection Rates?
Friday, April 21, 2023
James Harrop, MD, MSQHS
Professor
Jefferson Health
Philadelphia, Pennsylvania, United States
ePoster Presenter(s)
Introduction: Preoperative opioid use and increased postoperative infection rates have been shown to correlate1,2, but the mechanisms are unclear. Opiate medications have varying degrees of immunosuppressive properties. This study sought to assess whether the immunosuppressive properties of certain opioids play a role in the postoperative spinal infection rates.
Methods: A retrospective cohort study was performed using the Optum Pan-Therapeutic Electronic Health Records database. Adult patients who had their first lumbar fusion between 2015 to 2018 had 90-day preoperative opioid uses, and 2-year postoperative measurements available were included in the analysis. Patients were categorized into two groups based on consumption of opioid medications and these medications’ immunosuppressive abilities. 3-5 (includes fentanyl) versus non-immunosuppressive (includes oxycodone). Opioid dosage was measured as a daily morphine equivalent dose (MED). Cumulative infection incidence, adjusted for confounders including patient characteristics, and the risk (incidence) difference for the two groups was estimated. Statistical analysis was performed
Results: A total of 2,112 patients were enrolled in this study, among whom 1,275 patients were excluded as they either took both categories of opioids (77 patients) or did not take opioids that fell into either category (1,198 patients). The remaining 837 patients were identified as either immunosuppressive (12.8%) or non-immunosuppressive (87.2%) opioid users. The mean (standard deviation, median) opioid doses of the immunosuppressive and non-immunosuppressive groups were 52.6 (139.8, 32.4) mg/day and 57.5 (63.8, 45) mg/day MED, respectively. The confounder-adjusted risk of infections showed a statistically non-significant trend to be higher in the immunosuppressive group (13.7%) compared to the non-immunosuppressive group (12.5%) (P=0.725).
Conclusion : This study showed a trend of a higher rate of infections in patients using opioids with immunosuppressive properties. A larger cohort study and consideration of other drug properties are warranted to better understand the effects of opioids on spinal surgery outcomes.
Methods: A retrospective cohort study was performed using the Optum Pan-Therapeutic Electronic Health Records database. Adult patients who had their first lumbar fusion between 2015 to 2018 had 90-day preoperative opioid uses, and 2-year postoperative measurements available were included in the analysis. Patients were categorized into two groups based on consumption of opioid medications and these medications’ immunosuppressive abilities. 3-5 (includes fentanyl) versus non-immunosuppressive (includes oxycodone). Opioid dosage was measured as a daily morphine equivalent dose (MED). Cumulative infection incidence, adjusted for confounders including patient characteristics, and the risk (incidence) difference for the two groups was estimated. Statistical analysis was performed
Results: A total of 2,112 patients were enrolled in this study, among whom 1,275 patients were excluded as they either took both categories of opioids (77 patients) or did not take opioids that fell into either category (1,198 patients). The remaining 837 patients were identified as either immunosuppressive (12.8%) or non-immunosuppressive (87.2%) opioid users. The mean (standard deviation, median) opioid doses of the immunosuppressive and non-immunosuppressive groups were 52.6 (139.8, 32.4) mg/day and 57.5 (63.8, 45) mg/day MED, respectively. The confounder-adjusted risk of infections showed a statistically non-significant trend to be higher in the immunosuppressive group (13.7%) compared to the non-immunosuppressive group (12.5%) (P=0.725).
Conclusion : This study showed a trend of a higher rate of infections in patients using opioids with immunosuppressive properties. A larger cohort study and consideration of other drug properties are warranted to better understand the effects of opioids on spinal surgery outcomes.
