Surgical Resection of Glioblastoma in Patients ≥ 80 Years of Age: An Analysis of Overall Survival Outcomes Using the National Cancer Database
Friday, April 21, 2023
Julian Gendreau, MD
Researcher
Department of Neurological Surgery, Johns Hopkins School of Medicine
Baltimore, Maryland, United States
ePoster Presenter(s)
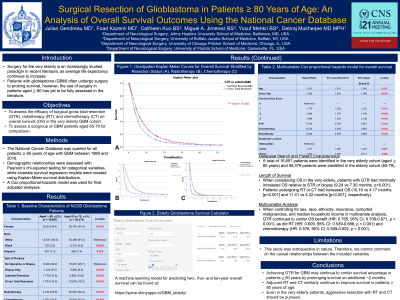
Introduction: Surgery for the very-elderly is an increasingly studied paradigm in recent literature, as average life expectancy continues to increase. Using the National Cancer Database, the authors aim to assess the efficacy of surgical resection, radiotherapy (RT), and chemotherapy (CT) on overall survival (OS) in the very-elderly GBM cohort while assessing a subgroup of GBM patients aged 65-79 for comparison.
Methods: The National Cancer Database was queried for all patients ≥ 65 years of age with GBM between 1989 and 2016. Demographic relationships were assessed with Pearson’s chi-squared testing for categorical variables, while bivariate survival regression models were created using Kaplan-Meier survival distributions. A Cox proportional-hazards model was used for final adjusted analyses.
Results: A total of 16,657 patients were identified in the very-elderly cohort (aged ≥ 80 years) while 59,379 patients were identified in the elderly cohort (65-79). Among very-elderly patients, 1,753 (10.5%) achieved GTR, 4,274 (25.6.%) received RT, and 3,071 (18.4%) received CT. When considering OS in the very-elderly, patients with GTR had minimally increased OS relative to STR or biopsy (9.24 vs 7.30 months, p< 0.001). Patients undergoing RT or CT had increased OS (10.16 vs 4.17 months and 11.41 vs 4.32 months, respectively; p< 0.001). Patients without loss of heterozygosity (LOH) on chromosome 19q had minimally increased OS (5.10 vs 5.71 months, p< 0.001). When controlling for sex, race, ethnicity, insurance, comorbid malignancies, and median household income in multivariate analysis, GTR continued to confer OS benefit (HR: 0.765, p < 0.001), as did radiotherapy (HR: 0.609, p < 0.001) and chemotherapy (HR: 0.576, p < 0.001).
Conclusion : Achieving GTR for GBM may continue to confer survival advantage in patients ≥ 80 years by prolonging survival an additional ~2 months. Patients ≥ 80 years of age should still be considered for safe but aggressive surgical resection and adjuvant therapy.
Methods: The National Cancer Database was queried for all patients ≥ 65 years of age with GBM between 1989 and 2016. Demographic relationships were assessed with Pearson’s chi-squared testing for categorical variables, while bivariate survival regression models were created using Kaplan-Meier survival distributions. A Cox proportional-hazards model was used for final adjusted analyses.
Results: A total of 16,657 patients were identified in the very-elderly cohort (aged ≥ 80 years) while 59,379 patients were identified in the elderly cohort (65-79). Among very-elderly patients, 1,753 (10.5%) achieved GTR, 4,274 (25.6.%) received RT, and 3,071 (18.4%) received CT. When considering OS in the very-elderly, patients with GTR had minimally increased OS relative to STR or biopsy (9.24 vs 7.30 months, p< 0.001). Patients undergoing RT or CT had increased OS (10.16 vs 4.17 months and 11.41 vs 4.32 months, respectively; p< 0.001). Patients without loss of heterozygosity (LOH) on chromosome 19q had minimally increased OS (5.10 vs 5.71 months, p< 0.001). When controlling for sex, race, ethnicity, insurance, comorbid malignancies, and median household income in multivariate analysis, GTR continued to confer OS benefit (HR: 0.765, p < 0.001), as did radiotherapy (HR: 0.609, p < 0.001) and chemotherapy (HR: 0.576, p < 0.001).
Conclusion : Achieving GTR for GBM may continue to confer survival advantage in patients ≥ 80 years by prolonging survival an additional ~2 months. Patients ≥ 80 years of age should still be considered for safe but aggressive surgical resection and adjuvant therapy.
