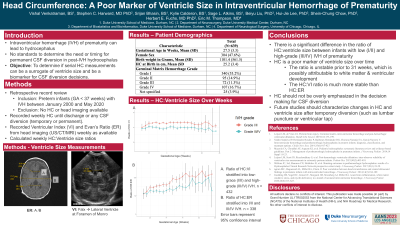
Tracking Head Circumference and Ventricular Size in Neonates with Intraventricular Hemorrhage of Prematurity
Friday, April 21, 2023
Vishal Venkatraman, BS (he/him/his)
Medical Student
Duke University
Durham, North Carolina, United States
ePoster Presenter(s)
Introduction: Intraventricular hemorrhage (IVH) of prematurity can lead to hydrocephalus, sometimes necessitating permanent cerebrospinal fluid (CSF) diversion via ventriculoperitoneal shunt or third ventriculostomy. Diversion is often decided via increasing head circumference (HC) or ventricular size measurements. Some patients receive temporary diversion, which can predict the need for permanent diversion in higher severity bleeds. We sought to characterize the conversion of temporary to permanent CSF diversion and if HC measurements in IVH correlated with the ventricular Evan’s Ratio (ER).
Methods: We queried the medical record for preterm infants with IVH born between January 2000 and May 2020 and collected demographics, procedures, weekly HC, and ER (ratio of maximum width of the frontal horns to inner width of the skull) from ultrasound, CT, or MRI from birth to discharge or permanent CSF diversion. The association between temporary and permanent CSF diversion was determined with Fisher’s exact test and HC/ER correlations were reported with Pearson’s coefficient.
Results: 641 patients with at least one HC measurement were included, of whom 73 (11.4%) had temporary diversion while 67 (10.5%) required permanent diversion. Temporary and permanent diversion were significantly associated across IVH Grades I (p=0.018), II (p < 0.001), III (p < 0.001), and IV (p < 0.001). Patients with permanent diversion showed a positive correlation between initial ER and HC (r=0.41, p=0.001). Infants born after 30 weeks gestational age showed correlation between initial HC and ER(r=0.37, p=0.001), while those before before 30 weeks didn't (r=0.02, p=0.75),
Conclusion : Temporary diversion is associated with the need for permanent diversion. Patients with CSF diversion showed a correlation between initial HC and ER, suggesting that those with high initial values of both be followed closely for potential intervention. Before 30 weeks gestational age, there is a poor correlation of HC and ER suggesting HC may not be a useful surrogate for ventricular size.
Methods: We queried the medical record for preterm infants with IVH born between January 2000 and May 2020 and collected demographics, procedures, weekly HC, and ER (ratio of maximum width of the frontal horns to inner width of the skull) from ultrasound, CT, or MRI from birth to discharge or permanent CSF diversion. The association between temporary and permanent CSF diversion was determined with Fisher’s exact test and HC/ER correlations were reported with Pearson’s coefficient.
Results: 641 patients with at least one HC measurement were included, of whom 73 (11.4%) had temporary diversion while 67 (10.5%) required permanent diversion. Temporary and permanent diversion were significantly associated across IVH Grades I (p=0.018), II (p < 0.001), III (p < 0.001), and IV (p < 0.001). Patients with permanent diversion showed a positive correlation between initial ER and HC (r=0.41, p=0.001). Infants born after 30 weeks gestational age showed correlation between initial HC and ER(r=0.37, p=0.001), while those before before 30 weeks didn't (r=0.02, p=0.75),
Conclusion : Temporary diversion is associated with the need for permanent diversion. Patients with CSF diversion showed a correlation between initial HC and ER, suggesting that those with high initial values of both be followed closely for potential intervention. Before 30 weeks gestational age, there is a poor correlation of HC and ER suggesting HC may not be a useful surrogate for ventricular size.
