Venous Thromboembolism in Aneurysmal Subarachnoid Hemorrhage: Risk Factors and Optimal Timing of Heparin Prophylaxis
Friday, April 21, 2023
Risheng Xu, MD PhD
Assistant Professor of Neurosurgery
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
ePoster Presenter(s)
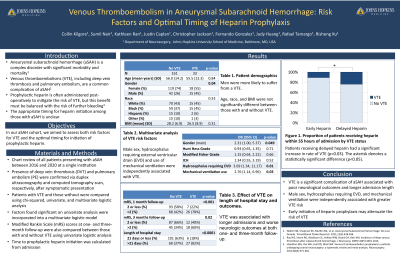
Introduction: Venous thromboembolism (VTE) is a significant contributor to morbidity and mortality among patients recovering from aneurysmal subarachnoid hemorrhage (aSAH). Prophylactic heparin reduces the risk of VTE, but the optimal timing for its initiation among aSAH patients remains unclear. We sought to assess risk factors for VTE and optimal timing of chemoprophylaxis in patients treated for aSAH.
Methods: From 2016 to 2020, 194 adult patients were treated for aSAH at our institution. Patient demographics, clinical diagnoses, complications, pharmacologic interventions, and outcomes were recorded. Risk factors for VTE were analyzed via Chi-squared, univariate, and multivariate regression.
Results: In total 33 patients presented with VTE (25 DVT, 14 PE). Patients with VTE had longer hospital stays (p < 0.0001) and worse outcomes and one-month (p=0.0003) and three-month follow-up (p= 0.02). Univariate predictors of VTE included male sex (p=0.03), neurologic presentation at admission (p=0.01-0.02), intracranial hemorrhage (p=0.03), hydrocephalus (p=0.005), external ventricular drain (EVD) placement (p < 0.001), and mechanical ventilation (p < 0.001). Only male sex (p=0.049), EVD (p=0.01) and ventilator (p=0.03) use remained significant upon multivariate analysis. Patients who received heparin more than 55 hours from admission were significantly more likely to sustain VTE (p=0.03).
Conclusion : Patients with aSAH are more likely to develop VTE following use of perioperative EVD or mechanical ventilation. VTE leads to longer hospital stays and worse outcomes among patients treated for aSAH. Delayed heparin initiation beyond 55 hours increases the risk of VTE. Our results may help guide surgical decision-making during recovery from aSAH and improve VTE-related postoperative outcomes.
Methods: From 2016 to 2020, 194 adult patients were treated for aSAH at our institution. Patient demographics, clinical diagnoses, complications, pharmacologic interventions, and outcomes were recorded. Risk factors for VTE were analyzed via Chi-squared, univariate, and multivariate regression.
Results: In total 33 patients presented with VTE (25 DVT, 14 PE). Patients with VTE had longer hospital stays (p < 0.0001) and worse outcomes and one-month (p=0.0003) and three-month follow-up (p= 0.02). Univariate predictors of VTE included male sex (p=0.03), neurologic presentation at admission (p=0.01-0.02), intracranial hemorrhage (p=0.03), hydrocephalus (p=0.005), external ventricular drain (EVD) placement (p < 0.001), and mechanical ventilation (p < 0.001). Only male sex (p=0.049), EVD (p=0.01) and ventilator (p=0.03) use remained significant upon multivariate analysis. Patients who received heparin more than 55 hours from admission were significantly more likely to sustain VTE (p=0.03).
Conclusion : Patients with aSAH are more likely to develop VTE following use of perioperative EVD or mechanical ventilation. VTE leads to longer hospital stays and worse outcomes among patients treated for aSAH. Delayed heparin initiation beyond 55 hours increases the risk of VTE. Our results may help guide surgical decision-making during recovery from aSAH and improve VTE-related postoperative outcomes.
