The impact of neurosurgical prehabilitation on postoperative patient outcomes: A systematic review
The Impact of Neurosurgical Prehabilitation on Postoperative Patient Outcomes: A Systematic Review
Friday, April 21, 2023
Emily M. Estes, BA (she/her/hers)
Medical Student
TTUHSC El Paso Paul L. Foster School of Medicine
El Paso, Texas, United States
ePoster Presenter(s)
Introduction: Prehabilitation (pre-operative rehabilitation) has been shown to improve functional capacity and post-operative outcomes in surgical patients. Diverse and tailored interventions, including exercise physiotherapy, nutritional optimization, and improved patient health, have the potential to improve neurosurgical outcomes. However, a paucity of literature exists related to neurosurgical prehabilitation. The goal of this systematic review is to assess the efficacy of prehabilitation on post-operative neurosurgical outcomes, including pain, functionality, and hospital stay length in patients undergoing neurosurgical procedures.
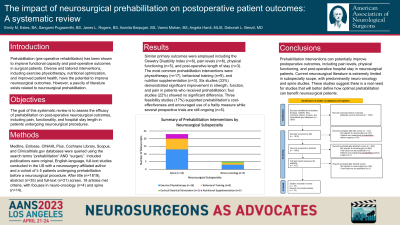
Methods: Medline, Embase, CINAHL Plus, Cochrane Library, Scopus, and Clinicaltrials.gov databases were queried using the search terms “prehabilitation” AND “surgery” (Fig. 1). Included publications were original, English-language, full-text studies conducted in the US with a neurosurgery-affiliated author and a cohort of ≥ 5 patients undergoing prehabilitation before a neurosurgical procedure. After title (n=1819), abstract (n=35) and full-text (n=21) screen, 18 articles met criteria, with focuses in neuro-oncology (n=4) and spine (n=14).
Results: Similar primary outcomes were employed including the Oswetry Disability Index (n=6), pain levels (n=6), physical functioning (n=5), and post-operative length of stay (n=3). The most common prehabilitation interventions were physiotherapy (n=17), behavioral training (n=9), and nutrition supplementation (n=3) (Fig. 2). Six studies (33%) demonstrated significant improvement in strength, function, and pain in patients who received prehabilitation; four studies (22%) showed no significant difference. Three feasibility studies (17%) supported prehabilitation’s cost-effectiveness and encouraged use of a frailty measure while several prospective trials are still ongoing (n=5).
Conclusion : Prehabilitation interventions can potentially improve postoperative outcomes, including pain levels, physical functioning, and post-operative hospital stay in neurosurgical patients. Current neurosurgical literature is extremely limited in subspecialty scope, with predominantly neuro-oncology and spine studies. These studies suggest there is a real need for studies that will better define how optimal prehabilitation can benefit neurosurgical patients.
Methods: Medline, Embase, CINAHL Plus, Cochrane Library, Scopus, and Clinicaltrials.gov databases were queried using the search terms “prehabilitation” AND “surgery” (Fig. 1). Included publications were original, English-language, full-text studies conducted in the US with a neurosurgery-affiliated author and a cohort of ≥ 5 patients undergoing prehabilitation before a neurosurgical procedure. After title (n=1819), abstract (n=35) and full-text (n=21) screen, 18 articles met criteria, with focuses in neuro-oncology (n=4) and spine (n=14).
Results: Similar primary outcomes were employed including the Oswetry Disability Index (n=6), pain levels (n=6), physical functioning (n=5), and post-operative length of stay (n=3). The most common prehabilitation interventions were physiotherapy (n=17), behavioral training (n=9), and nutrition supplementation (n=3) (Fig. 2). Six studies (33%) demonstrated significant improvement in strength, function, and pain in patients who received prehabilitation; four studies (22%) showed no significant difference. Three feasibility studies (17%) supported prehabilitation’s cost-effectiveness and encouraged use of a frailty measure while several prospective trials are still ongoing (n=5).
Conclusion : Prehabilitation interventions can potentially improve postoperative outcomes, including pain levels, physical functioning, and post-operative hospital stay in neurosurgical patients. Current neurosurgical literature is extremely limited in subspecialty scope, with predominantly neuro-oncology and spine studies. These studies suggest there is a real need for studies that will better define how optimal prehabilitation can benefit neurosurgical patients.
