Understanding associations between post-operative seizures and treatment course for patients with chronic SDH.
Understanding Associations Between Post-operative Seizures and Treatment Course for Patients with Chronic SDH
Friday, April 21, 2023

Kasuni Ranawaka (she/her/hers)
Medical Student
Geisel School of Medicine at Dartmouth
ePoster Presenter(s)
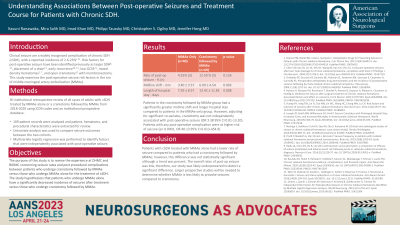
Introduction: Clinical seizures are recognized complications of chronic subdural hematomas (cSDH), with a reported incidence of 2.6-23%. Risk factors for post-operative seizures have been identified as larger SDH, placement of a drain, early recurrence, low GCS, mixed density hematomas, and open craniotomy with membranectomy. This study examines the post-operative seizure risk factors in the era of middle meningeal artery embolization (MMAe).
Methods: We conducted a bi-institutional retrospective review of all cases of adults with cSDH treated by MMAe alone (Group-A) or a craniotomy followed by MMAe (Group-B) from 2018-2020 using ICD9 codes and an institutional prospective database. 109 patient records were analyzed and patient, hematoma, and procedural characteristics were extracted for review. Univariate analysis was used to compare seizure outcomes between the two cohorts. Multivariate logistic regression was performed to identify factors that were independently associated with post-operative seizure.
Results: The overall rate of post-operative seizure was 7.34% (8 patients); 12.5% (5 patients) in Group-B, and 4.35% (3 patients) in Group-A. Patients Group-B had a significantly greater midline shift (6.09+/-4.54mm vs. 3.40+/-3.57mm, p = 0.003) and longer hospital stay (13.42+/-11.83 days vs. 7.59 +/-8.57 days, p = 0.008) compared to patients in Group-A. However, adjusting for significant co-variates, craniotomy was not independently associated with post-operative seizure (p=0.126, OR 3.38 95%CI 0.81-13.20). Patients with any post-operative complication were at higher risk of seizure (p < 0.0001, OR 40.13 95%CI 6.013-454.9).
Conclusion : Patients with cSDH treated with MMAe alone have a lower rate of seizure compared to patients who have craniotomy in addition to MMAe; however, this difference was not statistically significant although a trend was present. The overall rates of post-op seizure is low, therefore our study was likely underpowered to detect a significant difference. Larger prospective studies will be needed to determine whether MMAe is less likely to provoke seizures compared to craniotomy.
Methods: We conducted a bi-institutional retrospective review of all cases of adults with cSDH treated by MMAe alone (Group-A) or a craniotomy followed by MMAe (Group-B) from 2018-2020 using ICD9 codes and an institutional prospective database. 109 patient records were analyzed and patient, hematoma, and procedural characteristics were extracted for review. Univariate analysis was used to compare seizure outcomes between the two cohorts. Multivariate logistic regression was performed to identify factors that were independently associated with post-operative seizure.
Results: The overall rate of post-operative seizure was 7.34% (8 patients); 12.5% (5 patients) in Group-B, and 4.35% (3 patients) in Group-A. Patients Group-B had a significantly greater midline shift (6.09+/-4.54mm vs. 3.40+/-3.57mm, p = 0.003) and longer hospital stay (13.42+/-11.83 days vs. 7.59 +/-8.57 days, p = 0.008) compared to patients in Group-A. However, adjusting for significant co-variates, craniotomy was not independently associated with post-operative seizure (p=0.126, OR 3.38 95%CI 0.81-13.20). Patients with any post-operative complication were at higher risk of seizure (p < 0.0001, OR 40.13 95%CI 6.013-454.9).
Conclusion : Patients with cSDH treated with MMAe alone have a lower rate of seizure compared to patients who have craniotomy in addition to MMAe; however, this difference was not statistically significant although a trend was present. The overall rates of post-op seizure is low, therefore our study was likely underpowered to detect a significant difference. Larger prospective studies will be needed to determine whether MMAe is less likely to provoke seizures compared to craniotomy.
